Testicular Cancer
Risk Factors, Diagnosis & Cure
Testicular cancer is a rare but serious disease that mainly affects younger men and teenage boys. The most important thing to know about this cancer is that it is highly treatable. When found early, the chances of a complete cure are excellent.
Because it affects younger men who may not be thinking about cancer, it’s crucial to be aware of the signs and know what to look for. This guide will explain the risk factors, early signs, and treatment options for testicular cancer in simple, clear language, empowering you to take charge of your health.
Because it affects younger men who may not be thinking about cancer, it’s crucial to be aware of the signs and know what to look for. This guide will explain the risk factors, early signs, and treatment options for testicular cancer in simple, clear language, empowering you to take charge of your health.
Introduction to Testicular Cancer
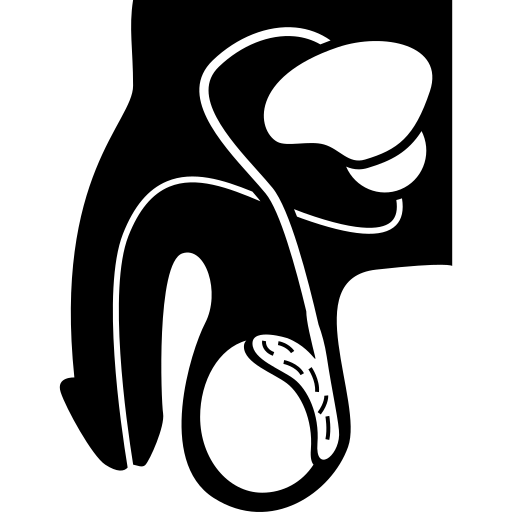
Testicular cancer happens when some cells in the testicles start growing in a way they shouldn’t. The testicles are part of the male body that make sperm and a hormone called testosterone. This cancer isn’t very common, but it usually affects boys and men between 15 and 40 years old. The great thing is that if doctors catch it early, most people get better.
Cancer Doctors first noticed testicular cancer in the 1700s, but treatments didn’t work very well back then. In the 1970s, scientists found a new medicine called cisplatin that helped a lot. Since then, better treatments and more people knowing the signs have made it much easier to cure this cancer. Today, testicular cancer is one of the easiest cancers to treat if caught early.
Have a Question?
Don’t let testicular problems go unnoticed. Get expert advice and understand your treatment options.
Types of Testicular Cancer
Testicular cancer is classified into several types, with the following four being the most common:
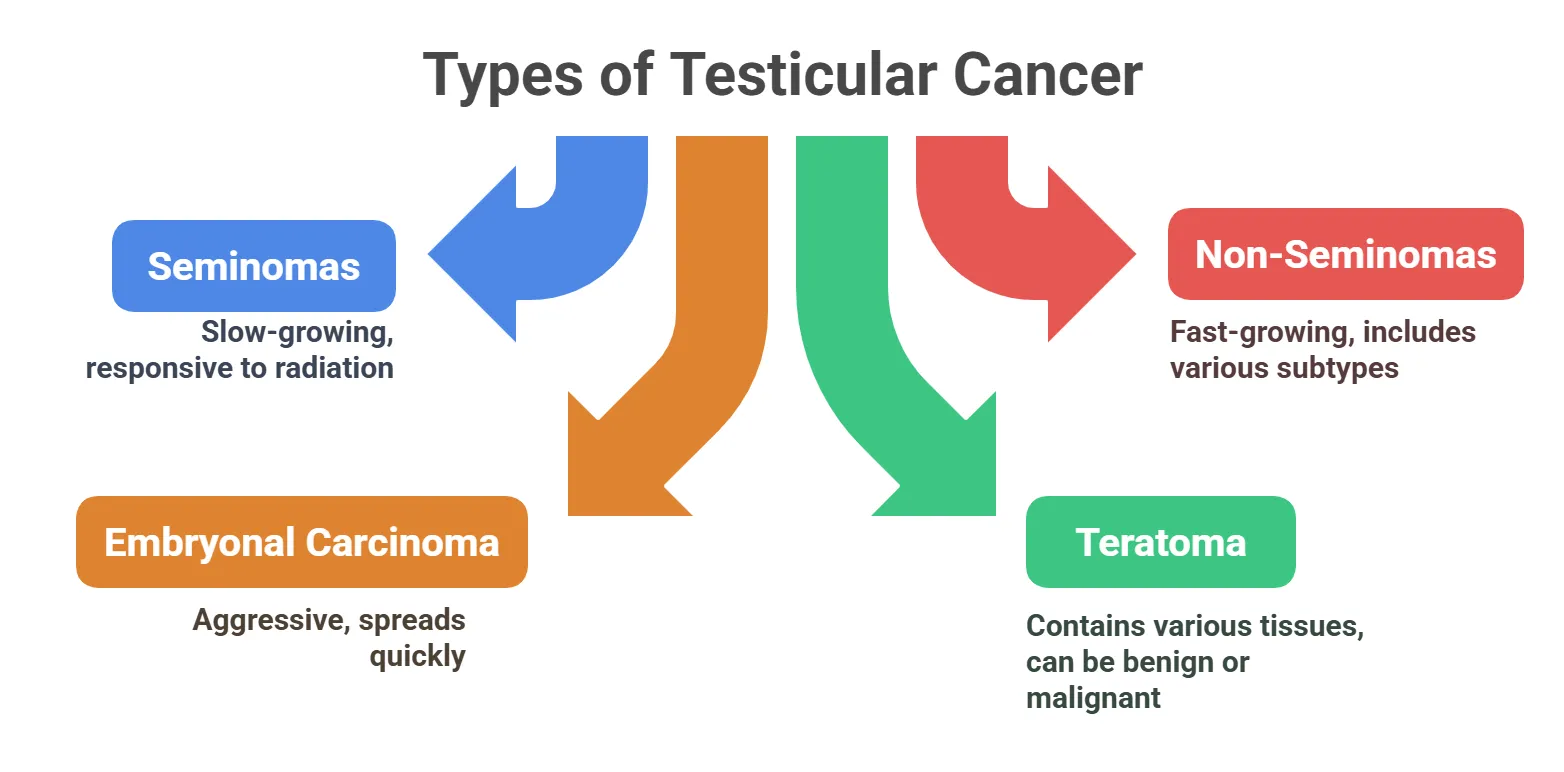
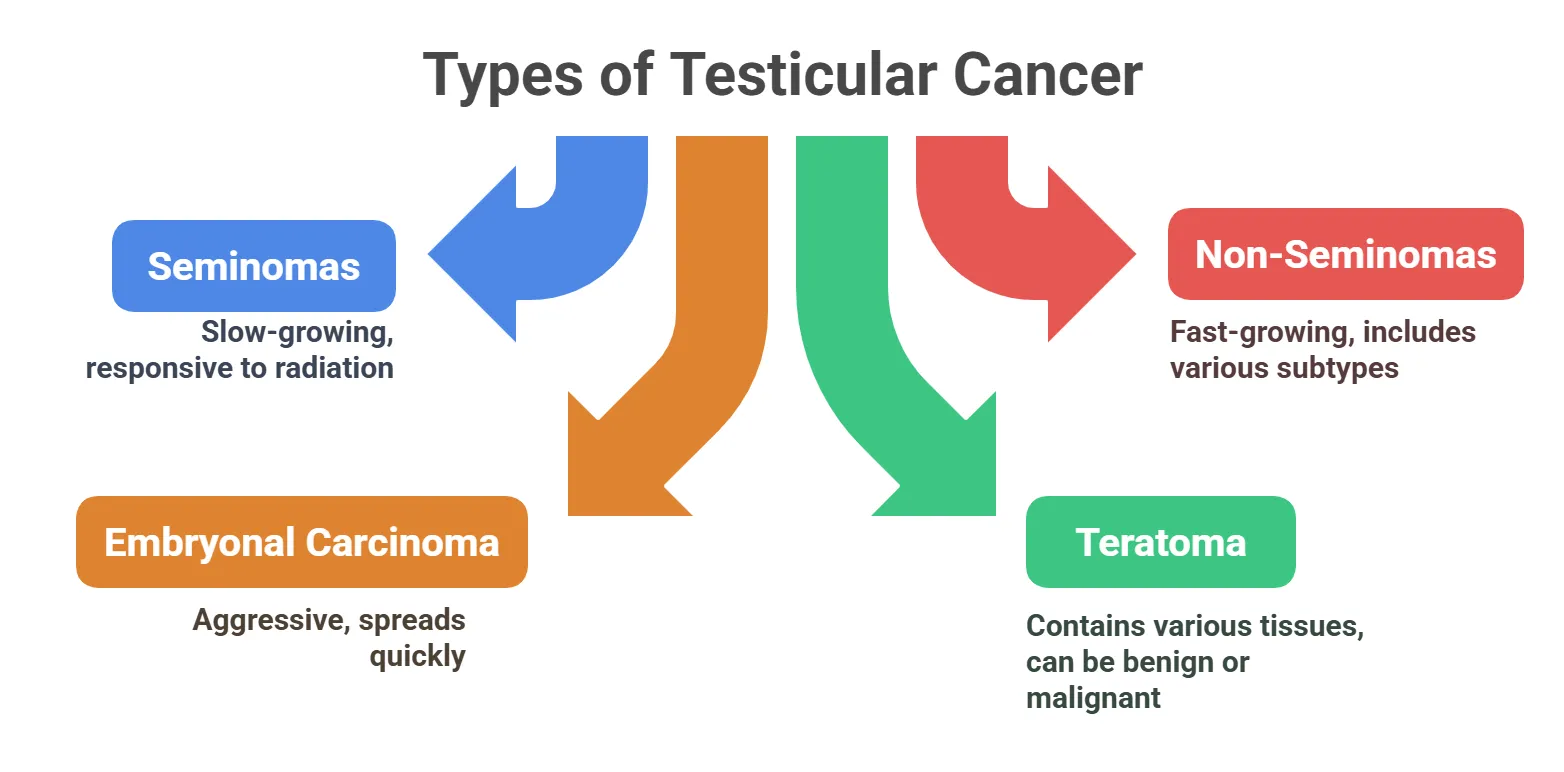
⦿ Seminomas: A type of germ cell tumor that tends to grow slowly. They are typically more responsive to radiation therapy.
⦿ Non-Seminomas: A group of germ cell tumors that grow more quickly. These include embryonal carcinoma, teratoma, choriocarcinoma, and yolk sac tumor.
⦿ Embryonal Carcinoma: An aggressive type of non-seminoma that can spread quickly. It often occurs with other types of germ cell tumors.
⦿ Teratoma: A type of non-seminoma containing different types of tissues. These can be mature (benign) or immature (malignant).
⦿ Non-Seminomas: A group of germ cell tumors that grow more quickly. These include embryonal carcinoma, teratoma, choriocarcinoma, and yolk sac tumor.
⦿ Embryonal Carcinoma: An aggressive type of non-seminoma that can spread quickly. It often occurs with other types of germ cell tumors.
⦿ Teratoma: A type of non-seminoma containing different types of tissues. These can be mature (benign) or immature (malignant).
Causes and Risk Factors of Testicular Cancer
The exact cause of testicular cancer is often unknown, but several risk factors can increase the likelihood of developing it.
- Undescended Testicle (Cryptorchidism)
This is the most significant risk factor, where one or both testicles don’t descend. Surgery can reduce but not eliminate the risk.
- Family History
Having a father or brother with testicular cancer increases your risk. Genetic factors may play a role in susceptibility.
- Age
Testicular cancer is most common in men aged 15 to 35. It is relatively rare after age 50.
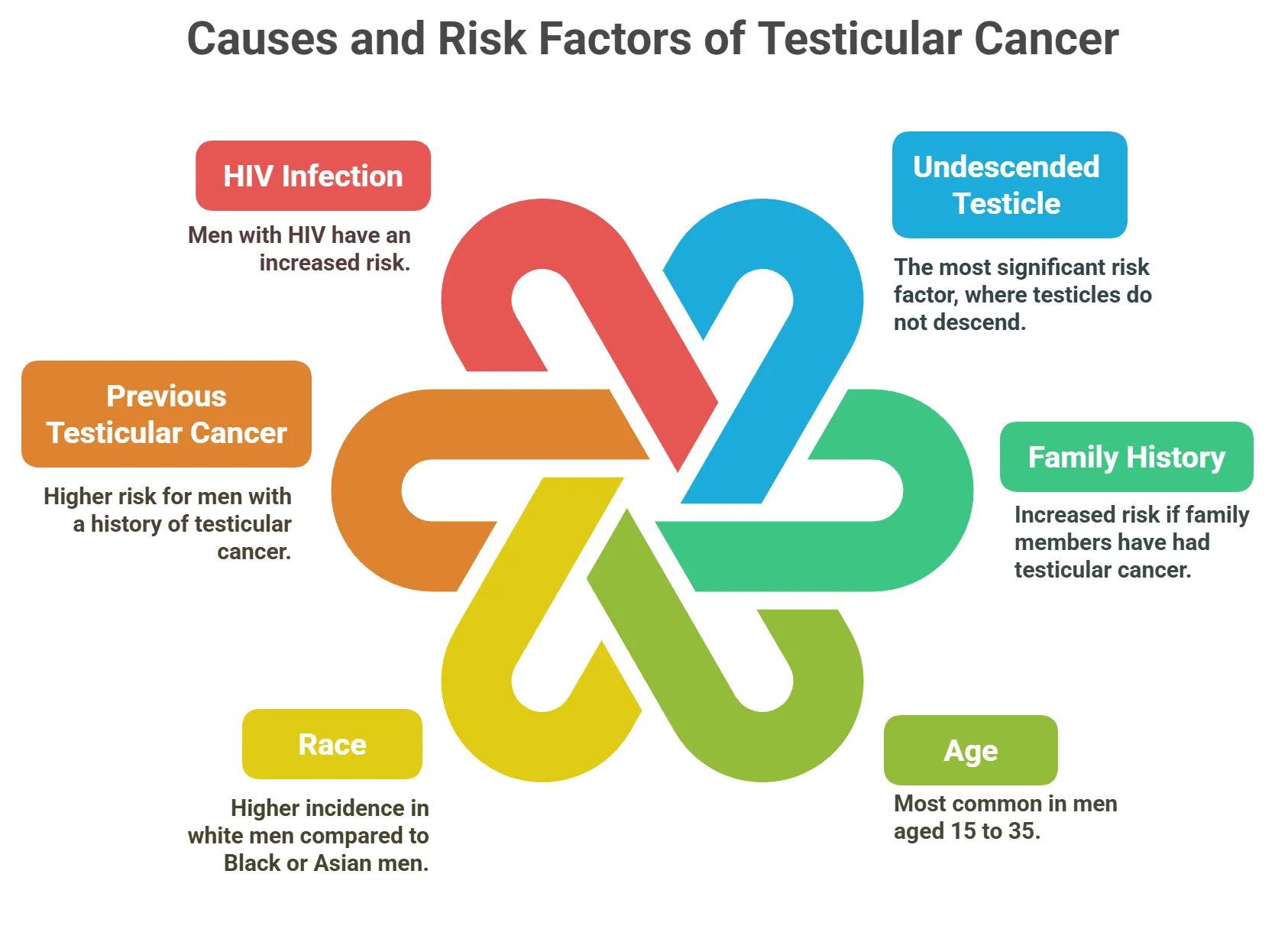
- Race
White men are more likely to develop testicular cancer than Black or Asian men. This disparity isn’t fully understood.
- Previous Testicular Cancer
Men who have had cancer in one testicle are at higher risk. The likelihood of developing cancer in the other testicle is increased.
Men with HIV have an increased risk of developing testicular cancer. The reasons for this association are still under investigation.
Testicular Cancer Symptoms
Recognizing the symptoms of testicular cancer is crucial for early detection and treatment.
Painless Lump or Swelling
The most common symptom is a lump in one testicle. It is usually painless but can sometimes cause discomfort.
Testicular Pain or Discomfort
Some men experience pain or a heavy sensation in the scrotum. This pain may be dull or sharp.

One testicle may become larger than the other. Any noticeable change in size should be checked by a doctor.
A persistent ache in the lower abdomen or groin area can occur. This can be a sign of cancer spread.
Fluid Collection in the Scrotum
Fluid may accumulate in the scrotum, causing swelling. This is known as a hydrocele.
Breast Tenderness or Growth
In rare cases, hormonal changes can cause breast tenderness. This is due to the cancer producing hormones.
Have a Question?
Are you experiencing any of these symptoms? Consult a seasoned specialist for appropriate diagnosis and management.
Diagnosis for Testicular Cancer
Diagnosing testicular cancer involves several tests to confirm the presence of cancer and determine its extent.
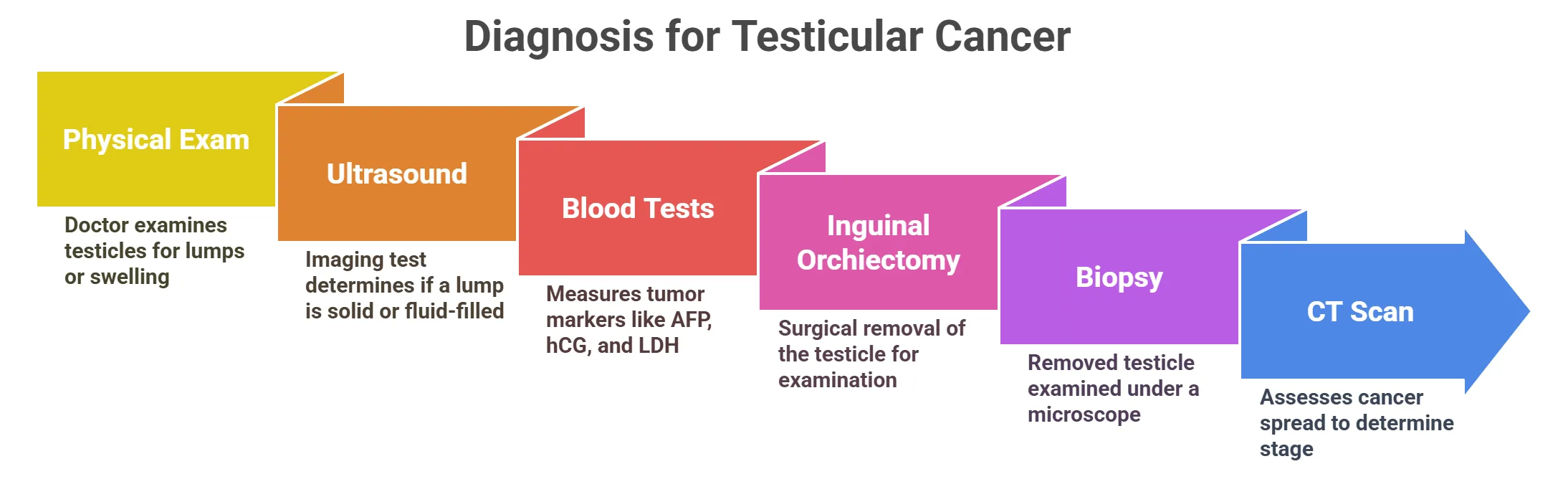
- Physical Exam
The doctor will examine the testicles for lumps or swelling. This is often the first step in detecting a potential issue.
This imaging test uses sound waves to create images of the testicles. It can help determine if a lump is solid or fluid-filled.
- Blood Tests
Blood tests measure tumor markers like AFP, hCG, and LDH. Elevated levels can indicate testicular cancer.
- Inguinal Orchiectomy
Surgical removal of the testicle for examination is often necessary. This helps confirm the diagnosis and type of cancer.
- Biopsy
A biopsy is typically not done before orchiectomy to avoid spreading the cancer. The removed testicle is examined under a microscope.
- CT Scan
CT scans of the abdomen, pelvis, and chest assess cancer spread. These scans help determine the stage of the cancer.
Treatment Options for Testicular Cancer
Testicular cancer is highly treatable, and treatment options depend on the type and stage of cancer.

Surgical removal of the affected testicle is a primary treatment. It can be the only treatment needed for early-stage cancer.

Uses high-energy rays to kill cancer cells, typically for seminoma types. It targets lymph nodes in the abdomen and pelvis.

Uses drugs to kill cancer cells throughout the body. It is often used for advanced or non-seminoma types of cancer.
Retroperitoneal Lymph Node Dissection (RPLND)
Surgery to remove lymph nodes in the abdomen. This is done if cancer has spread to these nodes.
Surveillance

Active monitoring with regular check-ups and tests. Used for early-stage cancer with a low risk of recurrence.
High-Dose Chemotherapy with Stem Cell Transplant

Involves high doses of chemo followed by a stem cell transplant. Reserved for advanced cases.
- Role of Radiotherapy in Testicular Cancer
Radiotherapy is used selectively in testicular cancer, depending on the type and stage. It is mainly effective in seminoma, one of the two main subtypes.
| Aspect | Details |
|---|---|
| When It Is Used |
- Mostly in Stage I or II seminoma - Rarely used in non-seminoma |
| Purpose |
- To kill remaining cancer cells after surgery - To treat lymph nodes (retroperitoneal) |
| How It Works | - Focused beams target specific areas where cancer might remain |
| Alternatives |
- Surveillance - Chemotherapy (especially in non-seminoma or advanced cases) |
| Side Effects |
- Fatigue - Nausea - Long-term risk of secondary cancers (low but present) |
Testicular Cancer Prevention
There’s no guaranteed way to prevent testicular cancer, but certain measures can help with early detection and managing risks.
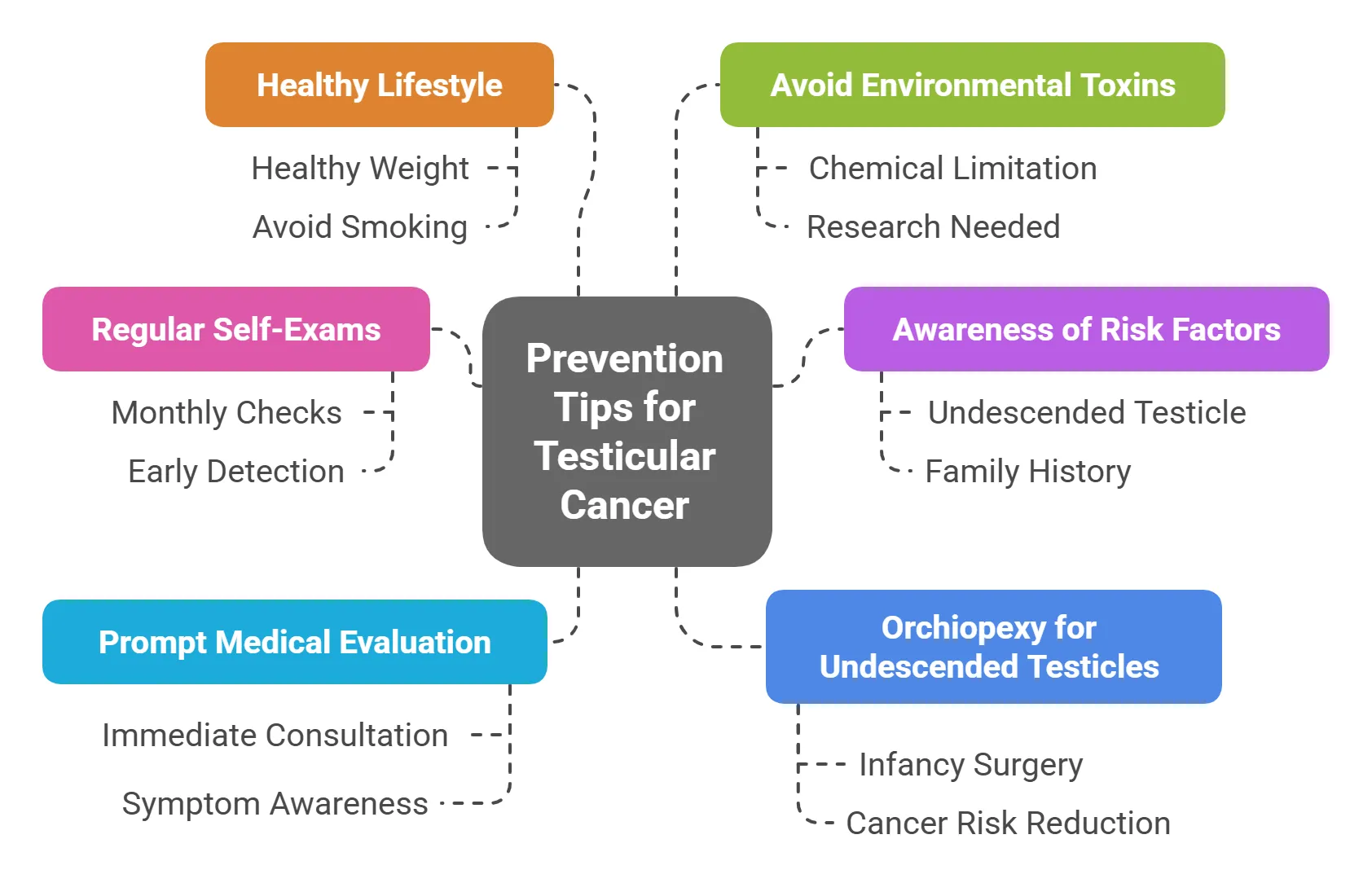
- Regular Self-Exams
Perform monthly self-exams to check for lumps or changes. Early detection improves treatment outcomes significantly.
- Awareness of Risk Factors
Know your risk factors, such as undescended testicle or family history. Discuss concerns with your doctor.
- Prompt Medical Evaluation
See a doctor if you notice any testicular changes or symptoms. Don’t delay seeking medical advice.
- Orchiopexy for Undescended Testicles
Surgery to correct an undescended testicle may reduce cancer risk. It is best performed in infancy.
Maintain a healthy weight and avoid smoking. A healthy lifestyle supports overall health.
- Avoid Environmental Toxins
Limit exposure to certain chemicals that may increase cancer risk. More research is needed in this area.
Have a Question?
Need help managing Testicular Cancer? Reach out to an expert and take control of your health today. Schedule an appointment today!
Frequently Asked Questions
What are the early signs of testicular cancer?
The most common sign is a painless lump or swelling in the testicle. Other symptoms can include a dull ache in the groin or lower abdomen.
How is testicular cancer diagnosed?
Diagnosis involves a physical examination, ultrasound, and blood tests to check for tumor markers. A biopsy is performed after the testicle is removed.
What are the risk factors for testicular cancer?
Risk factors include undescended testicles (cryptorchidism), family history, and being of Caucasian descent. Age (15-35) is also a factor.
What are the treatment options for testicular cancer?
Treatment options include surgery (orchiectomy), radiation therapy, and chemotherapy. The approach depends on the stage and type of cancer.
What is the survival rate for testicular cancer?
Testicular cancer has a very high survival rate, especially when detected early. Early detection and treatment significantly improve outcomes.
Can testicular cancer affect fertility?
Yes, treatment, especially surgery and chemotherapy, can affect fertility. Sperm banking before treatment is often recommended.
What are the symptoms of advanced testicular cancer?
Advanced testicular cancer may cause back pain, shortness of breath, or swelling in the legs, depending on where the cancer has spread.
Is testicular cancer hereditary?
While family history is a risk factor, most cases of testicular cancer are not hereditary.
What are tumor markers, and how are they used?
Tumor markers are substances in the blood that can indicate cancer. They help in diagnosis, staging, and monitoring treatment response.
Where can I find reliable information about testicular cancer?
Reliable information can be found at cancer organizations, medical websites, and by consulting with a healthcare professional. Always seek professional medical advice.

Written by
Dr. Swati Shah
MS, DrNB (Surgical Oncology)
Dr. Swati Shah is a Robotic Uro and Gynecological Cancer Surgeon in Ahmedabad.

Reviewed by
Dr. Harsh Shah
MS, MCh (G I cancer Surgeon)
Dr. Harsh Shah is a renowned GI and HPB Robotic Cancer Surgeon in Ahmedabad.
Last Updated on 6 months by Dr Harsh & Swati Shah
