Cervical Cancer
Diagnosis, Care & Recovery
But here is the most important thing to know: cervical cancer is one of the most preventable and treatable types of cancer. Most cases of this cancer are caused by a common virus called HPV (Human Papillomavirus). Because we know the cause, we can take steps to prevent it. Regular check-ups and screening tests are crucial for early detection and can save lives. This guide will explain everything you need to know in simple terms.
What is Cervical Cancer?
Have a Question?
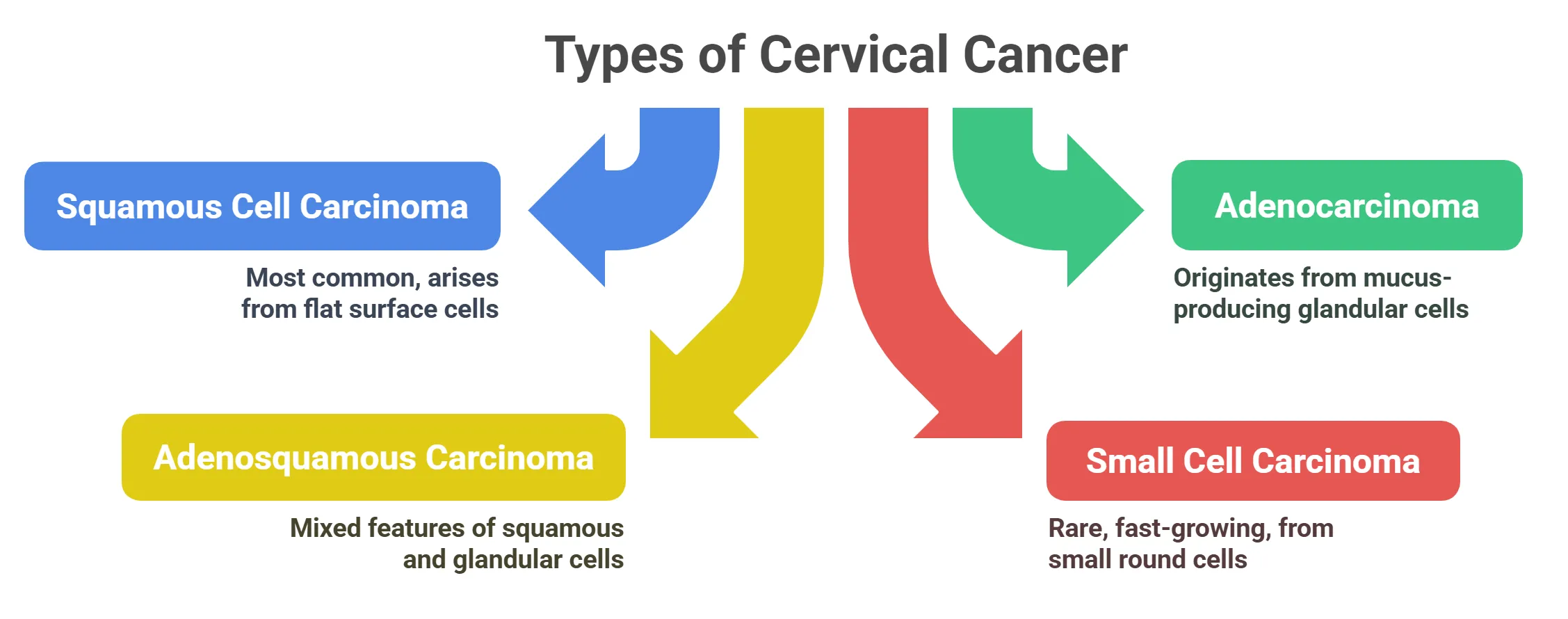
Types of Cervical Cancer
Cervical cancer starts in the cervix, which is the lower part of the uterus (womb). There are different types of cervical cancer, depending on the kind of cells that become cancerous. Here are the main types:
⦿ Adenocarcinoma: This type of cancer starts in the glandular cells of the cervix. These cells make mucus.
⦿ Adenosquamous Carcinoma: This is a mixed type of cancer. It has both squamous and glandular cell features.
⦿ Small Cell Carcinoma: This is a rare and fast-growing type of cervical cancer. It starts in small, round cells.
Early Signs and Symptoms of Cervical Cancer
- Common Symptoms
⦿ Between Periods: Bleeding between your regular periods.
⦿ After Intercourse: Bleeding after you have sex.
⦿ After Menopause: Any bleeding after you’ve gone through menopause (when your periods stop).
Unusual Vaginal Discharge
⦿ Color Changes: Discharge that is a different color than usual.
⦿ Odor Changes: Discharge that has a bad smell.
⦿ Consistency Changes: Discharge that is thicker or thinner than normal.
- Advanced Symptoms
Leg Pain

Swelling in Legs
Have a Question?
Risk Factors for Cervical Cancer
- Key Risk Factors
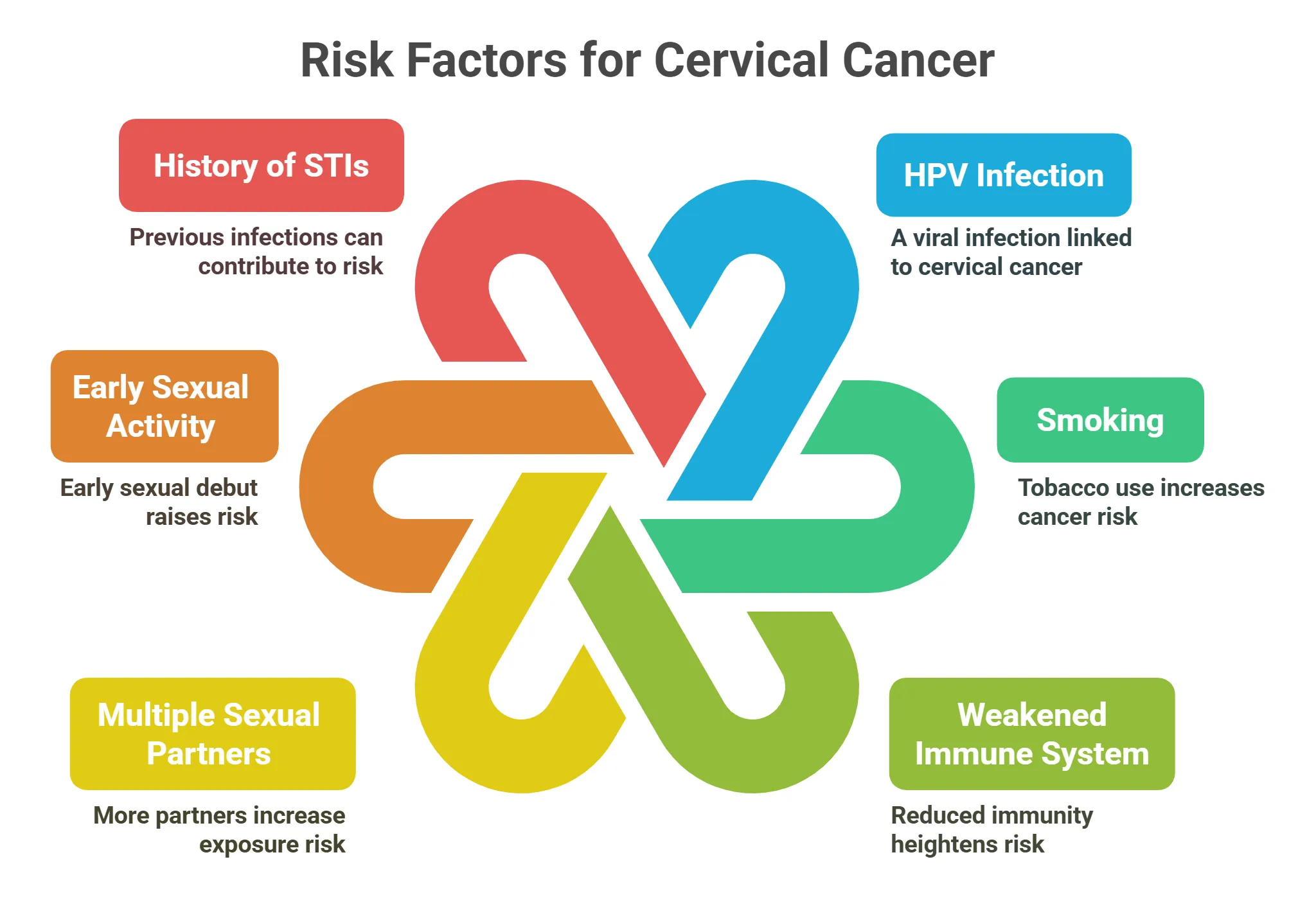
These are things that can increase your risk of getting cervical cancer.
⦿ HPV (Human Papillomavirus) Infection: The Primary Cause: HPV is a common virus that spreads through sexual contact. It is the main cause of cervical cancer.
⦿ Smoking: Increases Risk Significantly: Smoking makes you much more likely to get cervical cancer. Quitting smoking can lower your risk.
⦿ Weakened Immune System: If your immune system is weak, you are more likely to get cervical cancer. This can happen if you have HIV/AIDS or take drugs that suppress your immune system.
⦿ Multiple Sexual Partners: Having many sexual partners increases your risk of getting HPV.
⦿ Early Sexual Activity: Before Age 18: Starting to have sex before age 18 increases your risk of getting HPV.
⦿ History of STIs: Chlamydia, Gonorrhea: Having other sexually transmitted infections (STIs) can increase your risk of getting HPV.
⦿ Long-Term Use of Oral Contraceptives: Using birth control pills for a long time may slightly increase your risk.
- Non-Modifiable Risk Factors
⦿ Family History: Genetic Predisposition: If you have family members who had cervical cancer, your risk might be higher. Some genes can also increase your risk.
⦿ Age: Cervical cancer is most common between the ages of 30 and 50.
⦿ Race/Ethnicity: Cervical cancer is more common in certain racial and ethnic groups.
How is Cervical Cancer Diagnosed?
- Diagnostic Tests
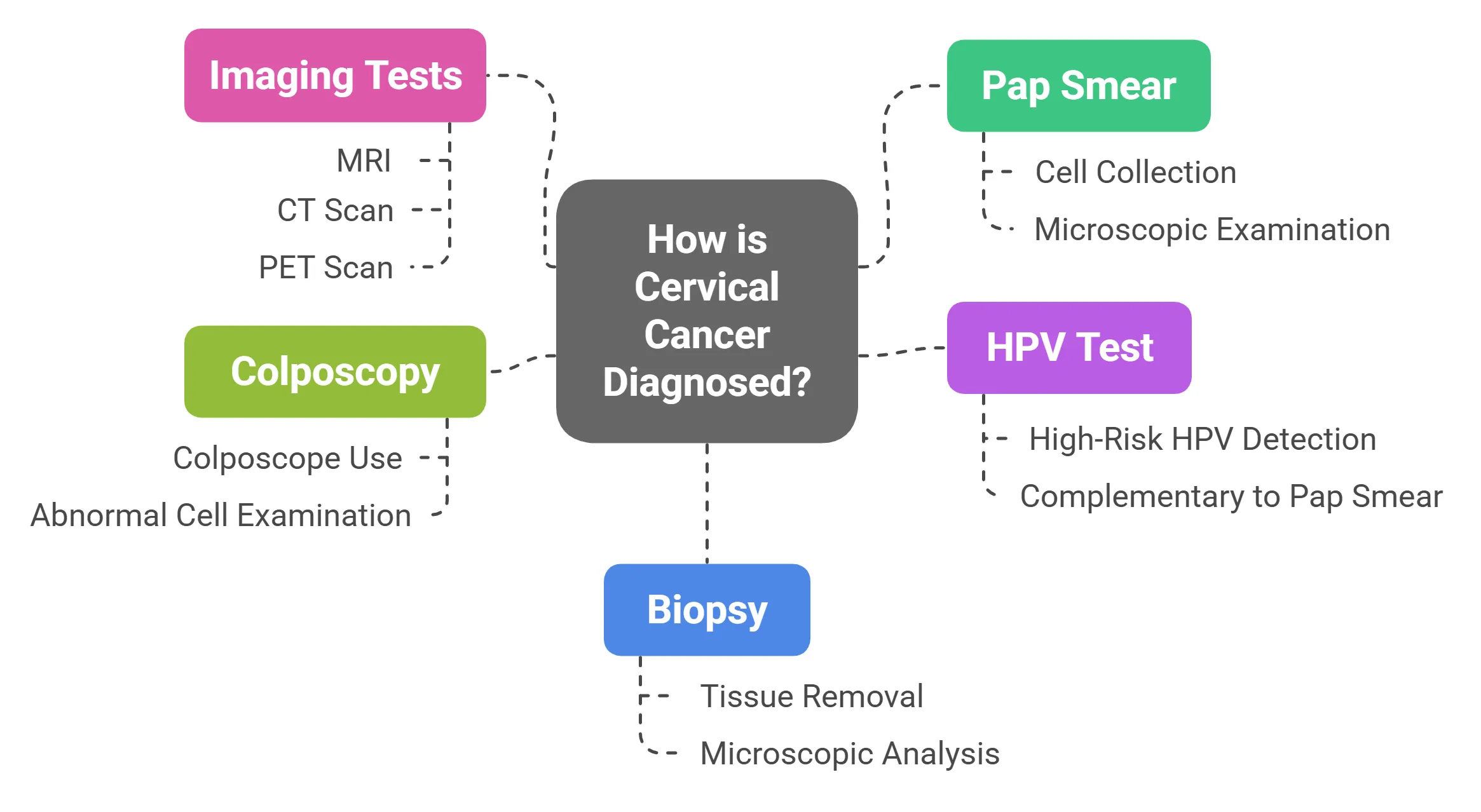
- Pap Smear: Screening for Abnormal Cells
- HPV Test: Detects High-Risk HPV Types
- Colposcopy: Visual Examination of the Cervix
- Biopsy: Confirming Cancer Cells
- Imaging Tests: MRI, CT Scan, PET Scan
If cancer is diagnosed, imaging tests may be done to see if the cancer has spread.
⦿ MRI (magnetic resonance imaging) uses magnets and radio waves to create detailed pictures of the body.
⦿ CT Scan (computed tomography) uses X-rays to create cross-sectional images.
⦿ PET Scan (positron emission tomography) uses a radioactive substance to look for cancer cells in the body.
Treatment Options for Cervical Cancer
- Surgical Treatments
Loop Electrosurgical Excision Procedure (LEEP): Removing Abnormal Tissue

Cone Biopsy: Removing a Cone-Shaped Piece of Cervical Tissue
Hysterectomy: Removing the Uterus
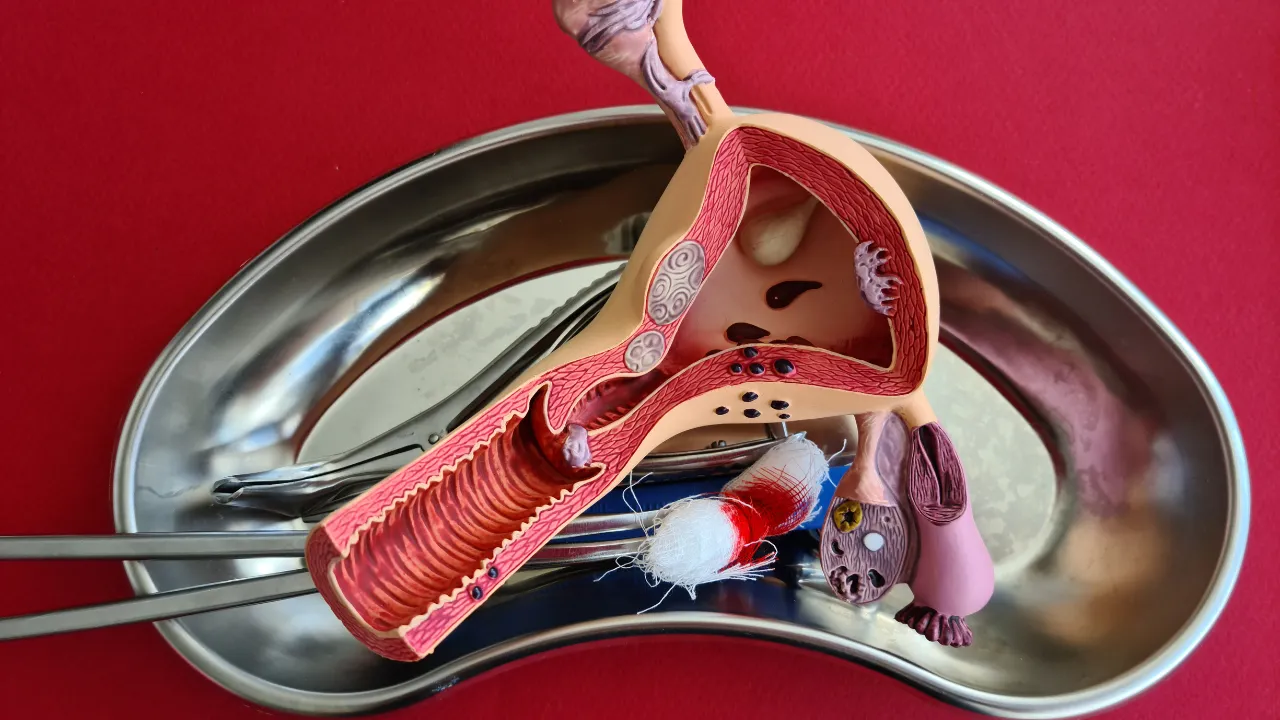
Radical Trachelectomy: Fertility-Sparing Surgery
Pelvic Exenteration: Removing the Cervix, Uterus, Vagina, and Other Organs

- Non-Surgical Treatments
Radiation Therapy: External Beam vs. Brachytherapy

Radiation therapy uses high-energy rays to kill cancer cells.
⦿ External beam radiation comes from a machine outside the body.
⦿ Brachytherapy involves placing radioactive material directly into the tumor.
Chemotherapy: Systemic Treatment

Targeted Therapy: Blocking Cancer Growth

Immunotherapy: Boosting the Immune System

- Comparison of Surgical vs Non-Surgical Treatments for Cervical Cancer
| Parameter | Surgical Treatment | Non-Surgical Treatment |
|---|---|---|
| Treatment Method | Cancer is removed from the body through an operation | Treatment using chemotherapy, radiation, or a combination of both |
| When It Is Used | In early stages (Stage I–IIA) when cancer is limited to the cervix | In advanced stages (IIB and beyond) or when surgery is not feasible |
| Advantages | Cancer is removed completely; treatment duration is usually shorter | Uterus may be preserved; no surgical risks; more options available |
| Risks / Side Effects | Bleeding, infection, anesthesia-related risks | Fatigue, hair loss, nausea, mouth ulcers, longer treatment time |
| Effect on Fertility | Pregnancy is not possible after uterus removal | Fertility may be preserved in some early-stage cases |
| Risk of Recurrence | Generally lower in well-selected cases | Depends on cancer stage and response to treatment |
Preventing Cervical Cancer
- Primary Prevention
⦿ HPV Vaccination: Recommended Ages and Benefits: The HPV vaccine protects against the types of human papillomavirus (HPV) that cause most cervical cancers. It is recommended for girls and boys, ideally before they become sexually active. The vaccine is most effective when given at younger ages.
⦿ Delaying Sexual Activity: Reducing HPV Exposure: Delaying the start of sexual activity can reduce the risk of HPV exposure, as HPV is primarily transmitted through sexual contact.
⦿ Limiting Sexual Partners: Limiting the number of sexual partners can decrease the risk of HPV infection. The more partners you have, the higher the chance of contracting HPV.
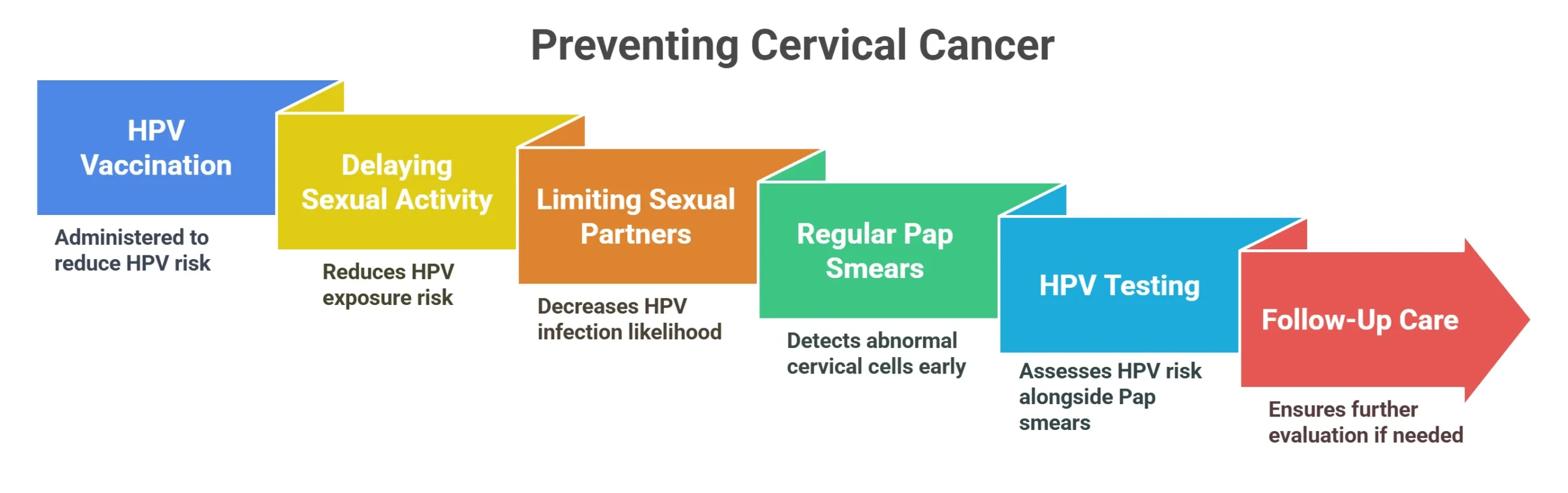
- Secondary Prevention
⦿ Regular Pap Smears: Starting at Age 21: Regular Pap smears are crucial for detecting abnormal cells in the cervix before they turn into cancer. It is generally recommended to start Pap smears at age 21, regardless of when you become sexually active.
⦿ HPV Testing: Guidelines and Recommendations: HPV testing can be done along with or instead of Pap smears, depending on your age and medical history. Guidelines vary, so talk to your doctor about the best screening schedule for you.
⦿ Follow-Up Care for Abnormal Results: If a Pap smear or HPV test comes back with abnormal results, it is important to follow up with your doctor for further evaluation and treatment, if necessary. This may include a colposcopy and biopsy.
Have a Question?
Schedule an appointment today!
Frequently Asked Questions
What is cervical cancer, and where does it start?
What are the main causes and risk factors for cervical cancer?
What are the common symptoms of cervical cancer?
How is cervical cancer usually diagnosed?
What are the different stages of cervical cancer?
What are the primary treatment options available for cervical cancer?
Can cervical cancer be cured, and what factors affect the chances of a cure?
How can cervical cancer be prevented?
What should I expect during and after cervical cancer treatment in terms of side effects and recovery?
Where can I get vaccinated against HPV in India?

Written by
Dr. Swati Shah
MS, DrNB (Surgical Oncology)
Dr. Swati Shah is a Robotic Uro and Gynecological Cancer Surgeon in Ahmedabad.

Reviewed by
Dr. Harsh Shah
MS, MCh (G I cancer Surgeon)
Dr. Harsh Shah is a renowned GI and HPB Robotic Cancer Surgeon in Ahmedabad.