Low Anterior Resection Surgery
Procedure, Recovery, and Life After
This detailed guide is designed to explain everything about Low Anterior Resection surgery in simple, easy-to-understand language. We will walk you through what the surgery is, why it’s done, what to expect before and after, and how you can live a full and healthy life following the procedure.
Summary
- What is Low Anterior Resection?
- When and How is it Done?
- Recovery, Benefits and Risks
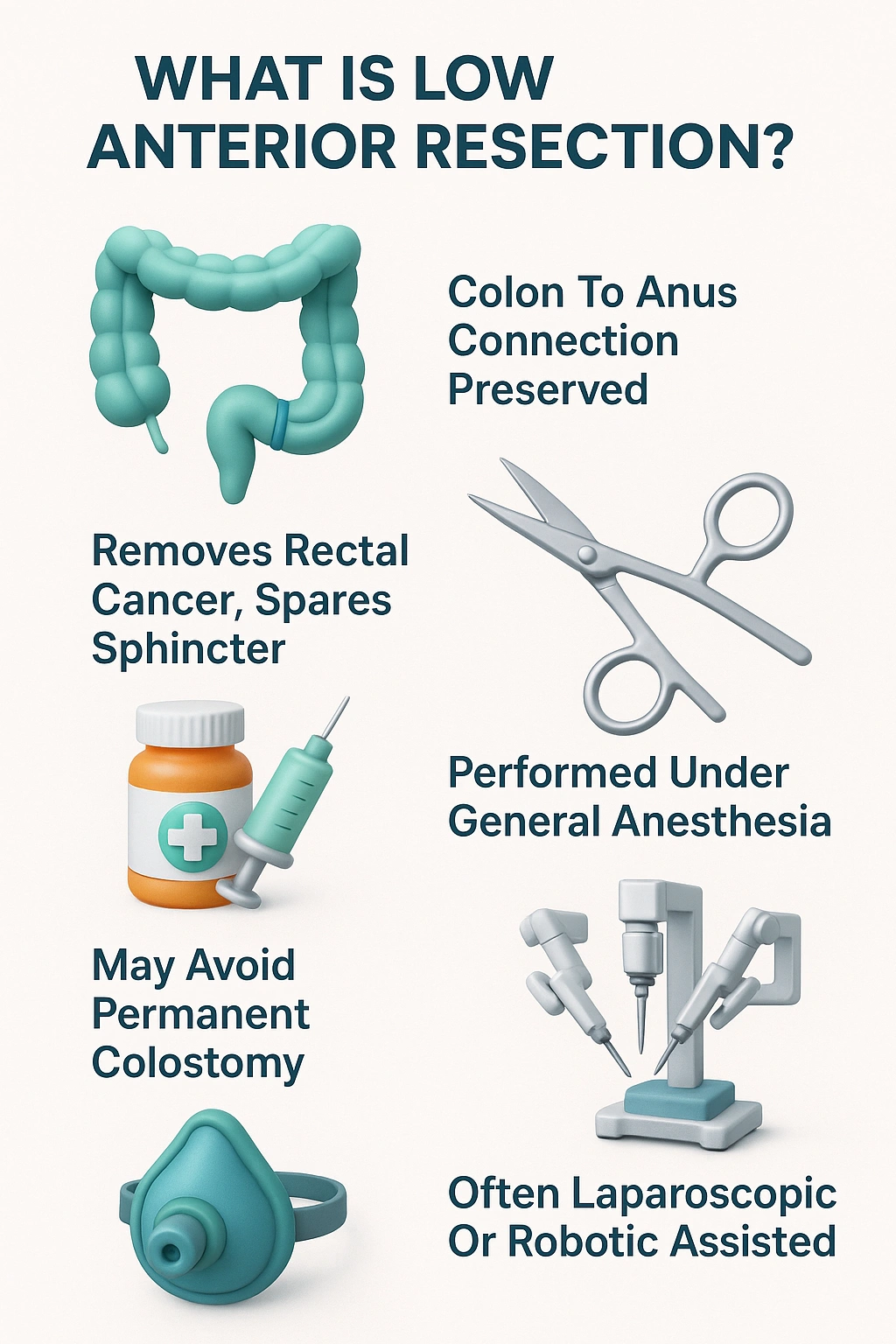
What Is Low Anterior Resection Surgery?
- History
- Overview of LAR Procedure
- Differences Between LAR and Other Rectal Surgeries
You may have heard of other rectal surgeries, like an Abdominoperineal Resection (APR). The biggest difference is what happens to the anus and the path of your stool.
⦿ Low Anterior Resection (LAR): In this surgery, the surgeon saves your anal sphincter muscles. These are the muscles that control when you pass stool. This means after you recover, you will be able to go to the toilet in the normal way.
⦿ Abdominoperineal Resection (APR): This surgery is usually for cancer very low in the rectum, close to the sphincter muscles. In an APR, the surgeon removes the rectum, anus, and sphincter muscles. This means a permanent colostomy (or stoma bag) is needed to collect stool.
- Importance of Sphincter Preservation in LAR
It allows you to avoid a permanent stoma, which is a major concern for many patients. This preservation is a key factor that makes Low Anterior Resection a preferred option whenever it is medically safe.
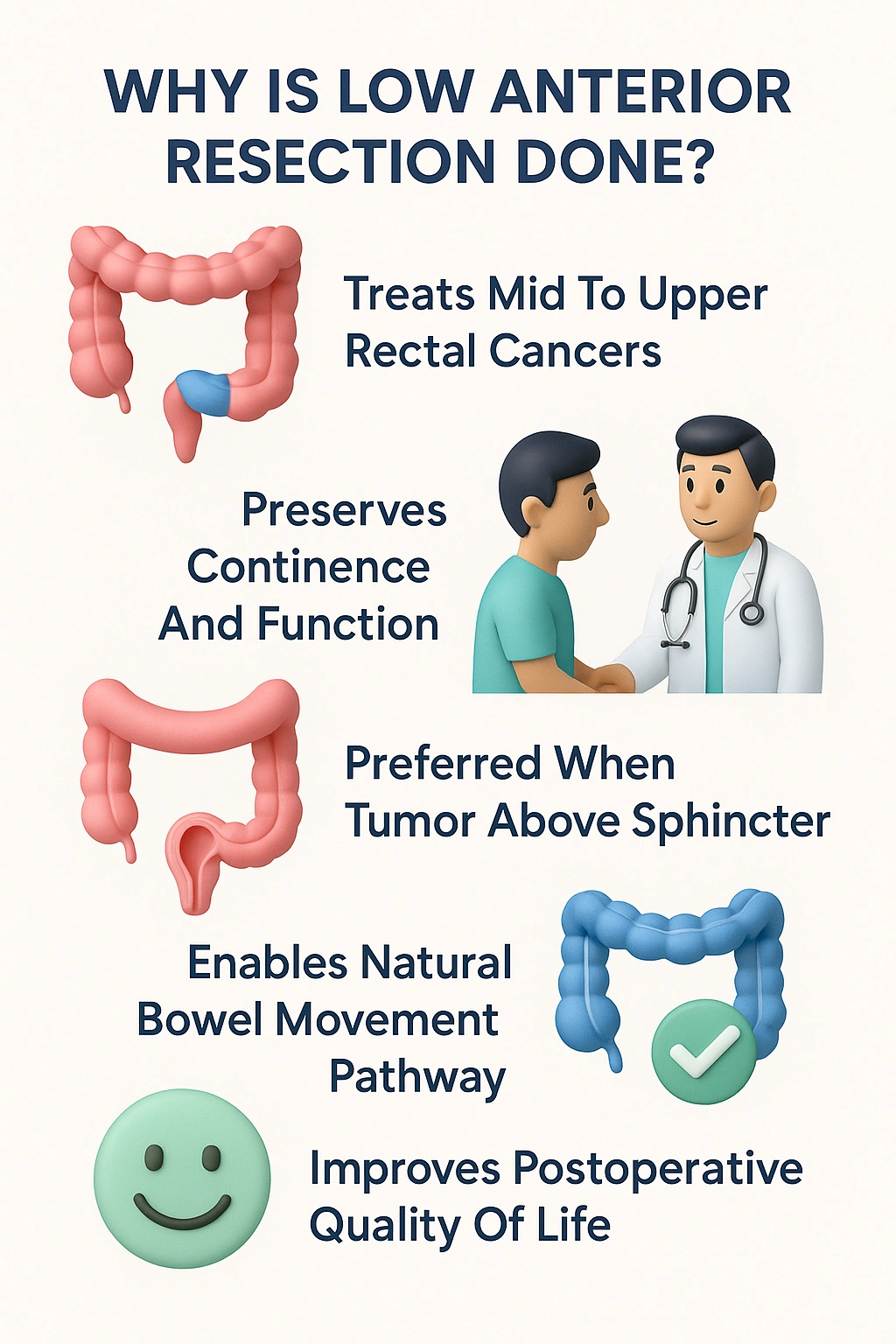
- Indications for Low Anterior Resection
Indications and Patient Selection
- Rectal Cancer: Upper and Mid-Rectum
- Benign Conditions Requiring LAR
While cancer is the main reason, LAR can also be used for some non-cancerous (benign) conditions. These are less common but can include:
⦿ Diverticulitis: Severe or complicated cases where small pouches in the intestinal wall become inflamed or infected.
⦿ Endometriosis: When tissue similar to the lining of the uterus grows on the rectum, causing severe pain or blockage.
⦿ Rectal Prolapse: A condition where the rectum slips out of place and protrudes from the anus.
- Criteria for Sphincter-Saving Surgery
⦿ Tumour Location: The tumour must be far enough from the sphincter muscles to allow for a “clear margin.” This means the surgeon can remove the tumour plus a border of healthy tissue around it to ensure no cancer cells are left behind.
⦿ Patient’s Sphincter Function: The patient must have good sphincter control before the surgery. If the muscles are already weak, saving them may not lead to good bowel control after the operation.
⦿ Overall Health: The patient needs to be healthy enough to undergo a major surgery and recover well.
- Factors Influencing Surgical Decision
Preoperative Assessment and Preparation
- Colonoscopy and Biopsy
- MRI and CT Scans for Staging
Once cancer is confirmed, the next step is to “stage” it. Staging means finding out the exact size of the tumour and if it has spread.
⦿ MRI (Magnetic Resonance Imaging): An MRI of the pelvis gives a very detailed picture of the rectum and the surrounding tissues. It helps the surgeon see how deep the tumour has grown and if it is close to other organs or the sphincter muscles.
⦿ CT (Computed Tomography) Scan: A CT scan of the chest, abdomen, and pelvis is used to check if the cancer has spread to distant organs like the liver or lungs.
- Bowel Preparation Protocols
Your bowel needs to be completely empty and clean before the surgery. This reduces the risk of infection. Your doctor will give you a specific “bowel prep” routine to follow in the days leading up to the operation. This usually involves:
⦿ Eating a low-fibre or liquid-only diet.
⦿ Drinking a special laxative solution that will cause you to have multiple bowel movements to clear out your intestines.
It’s not the most pleasant experience, but it is very important for your safety.
- Nutritional and Physical Optimization
Getting your body in the best possible shape before surgery can help you recover faster. This is sometimes called “prehabilitation.” It may include:
⦿ Eating a healthy, high-protein diet to build strength.
⦿ Doing gentle exercises, like walking, to improve your fitness.
⦿ Quitting smoking, as smoking can slow down healing and increase the risk of complications.
⦿ Managing other health issues, like diabetes or high blood pressure.
Steps of Low Anterior Resection Procedure
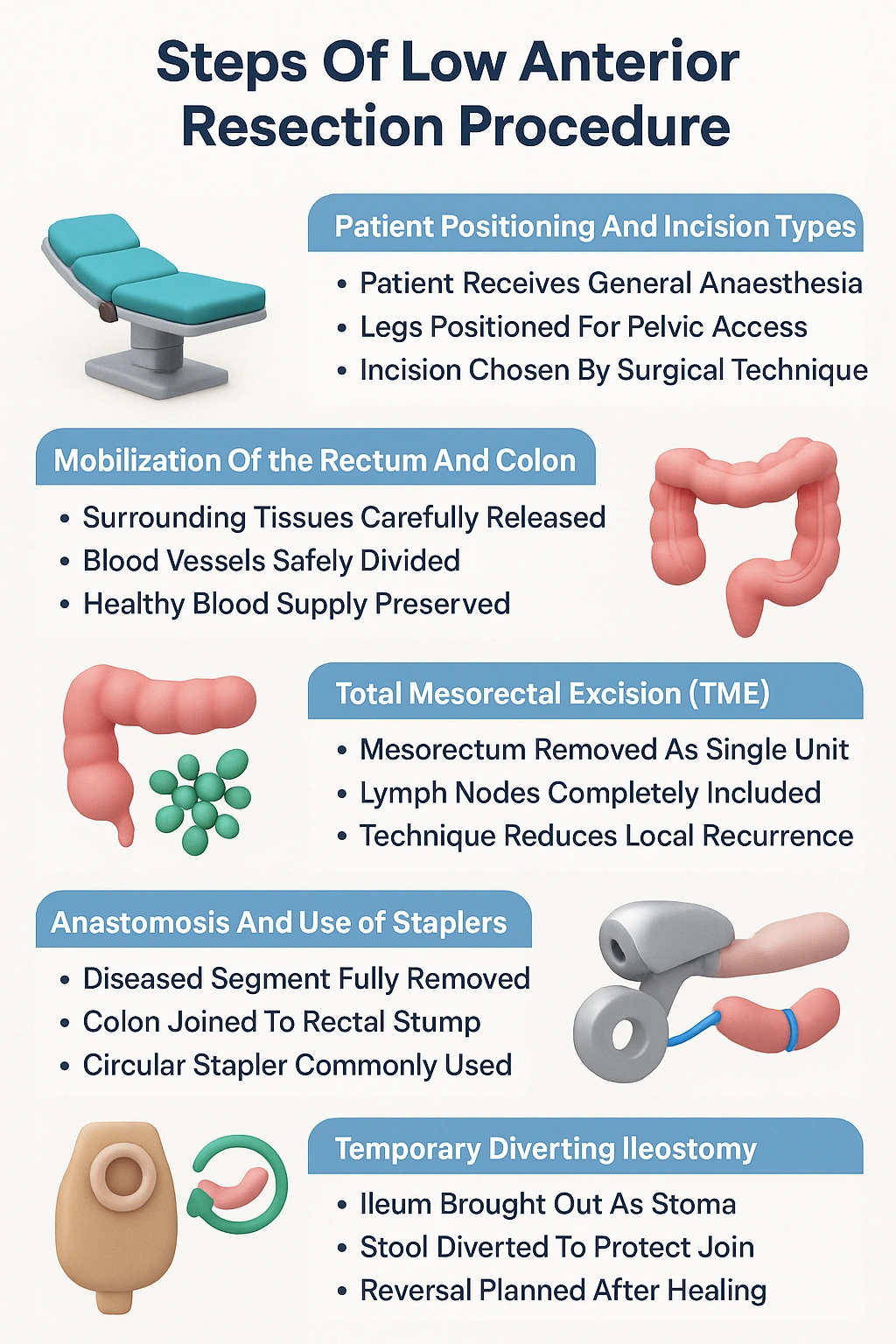
- Patient Positioning and Incision Types
You will be given general anaesthesia, so you will be completely asleep and feel no pain. You will be positioned on the operating table, usually with your legs raised, to give the surgeon the best access to the pelvic area.
The surgeon will then make an incision (a cut) to access your abdomen. The type of incision depends on the surgical technique being used (open, laparoscopic, or robotic).
- Mobilization of the Rectum and Colon
The surgeon first needs to free the colon and rectum from their surrounding tissues. This is called “mobilization.”
They will carefully cut the attachments and blood vessels connected to the section of the bowel that needs to be removed, making sure to preserve the blood supply to the parts that will remain.
- Total Mesorectal Excision (TME)
This is a critical part of the surgery for rectal cancer. The mesorectum is a fatty tissue that surrounds the rectum. It contains lymph nodes, which are small glands where cancer can spread.
During Total Mesorectal Excision (TME), the surgeon removes the rectum along with this entire fatty envelope as a single, intact package. This technique has been proven to significantly reduce the chances of the cancer coming back in the same area. This step is a standard part of a modern Low Anterior Resection for cancer.
- Anastomosis and Use of Staplers
After the diseased section is removed, the surgeon performs the anastomosis—the reconnection. The healthy end of the colon is brought down and joined to the remaining part of the rectum. In most cases, this is done using a special surgical stapler, which creates a neat and secure connection, shaped like a circle. Sometimes, the surgeon may use stitches (sutures) instead.
- Temporary Diverting Ileostomy (If Required)
In some cases, especially when the anastomosis is very low in the pelvis, the surgeon may decide to create a temporary “diverting ileostomy“. This is a procedure where the end of the small intestine (the ileum) is brought out through a small opening in your abdomen, called a stoma. Your stool will pass through this stoma into a bag that you wear on the outside.
This is done to protect the new connection (anastomosis) by diverting stool away from it while it heals. This is not permanent. The ileostomy is usually reversed in a second, smaller surgery a few months later, once the surgeon is sure the anastomosis has healed completely. Your doctor will discuss if this is likely in your case. A medical procedure like the anterior low resection requires careful planning for such possibilities.
Surgical Techniques: Open vs Laparoscopic vs Robotic
- Benefits of Minimally Invasive LAR
The benefits of minimally invasive surgery often include:
⦿ Less pain after the operation.
⦿ Smaller scars.
⦿ A shorter hospital stay.
⦿ Faster return to normal activities.
⦿ Less blood loss during surgery.
- Robotic Assistance in Pelvic Dissection
Robotic surgery is an advanced form of laparoscopic surgery. The surgeon sits at a console and controls robotic arms that hold the surgical instruments. The robotic system provides a high-definition, 3D view of the surgical area and allows for very precise movements. This is particularly helpful in the narrow, deep space of the pelvis where the rectum is located, making the delicate dissection of a Low Anterior Resection easier.
- Comparing Recovery and Outcomes
While minimally invasive approaches often lead to a quicker initial recovery, the long-term outcomes in terms of cancer control are generally considered to be the same as traditional open surgery when performed by an experienced surgeon.
- Swipe right to view the full table
| Feature | Open Surgery | Laparoscopic Surgery | Robotic Surgery |
|---|---|---|---|
| Incision | One long incision in the abdomen | Several small incisions (keyhole) | Several small incisions (keyhole) |
| Pain Level | Higher postoperative pain | Lower postoperative pain | Lower postoperative pain |
| Hospital Stay | Typically longer (5–10 days) | Typically shorter (3–7 days) | Typically shorter (3–7 days) |
| Recovery Time | Longer, several weeks to months | Faster, return to activities sooner | Faster, return to activities sooner |
| Surgeon's View | Direct view of the surgical site | 2D view on a monitor | High-definition, 3D view |
| Instrument Control | Direct hand control | Control of long, straight instruments | Control of wristed, highly flexible instruments |
Postoperative Recovery and Hospital Stay
- Pain Management and Early Mobilization
- Diet Progression and Bowel Function
- Swipe right to view the full table
| Stage | Allowed Foods | Foods to Avoid |
|---|---|---|
| First 1-2 Days | Clear liquids: Water, clear broth, juice, tea. Ice chips. | Solid foods, milk, and dairy products. |
| Days 3-5 | Full liquids and soft foods: Soup, yogurt, pudding, mashed potatoes, scrambled eggs. | High-fibre foods, raw vegetables, spicy foods, fried foods. |
| Weeks 2-4 | Gradually reintroduce a low-fibre diet. Small, frequent meals are best. | Hard-to-digest foods: Nuts, seeds, corn, popcorn, very fibrous vegetables. |
| Long-Term | Slowly increase fibre intake to find a balanced diet that works for you. Stay well-hydrated. | Foods that you notice cause gas, bloating, or diarrhea. This can be different for everyone. |
- Monitoring for Complications
- Discharge Planning and Follow-Up
You can usually go home after 3 to 7 days, depending on the type of surgery and how quickly you recover. Before you leave, your team will give you instructions on:
⦿ How to care for your incisions.
⦿ What you can eat and drink.
⦿ What activities are safe to do.
⦿ When to call the doctor.
You will have a follow-up appointment with your surgeon a few weeks after you go home to check on your healing. This is a vital part of the care after a Low Anterior Resection.
Possible Complications and Risks
- Anastomotic Leak
This can cause a severe infection (peritonitis) and may require another surgery. A temporary ileostomy is often created to reduce the risk of this happening.
- Bowel Dysfunction (Low Anterior Resection Syndrome)
This collection of symptoms is known as low anterior resection syndrome lars.
- Urinary and Sexual Dysfunction
The nerves that control bladder function and sexual function in both men and women are located very close to the rectum in the pelvis. During the surgery, these nerves can sometimes be bruised or damaged.
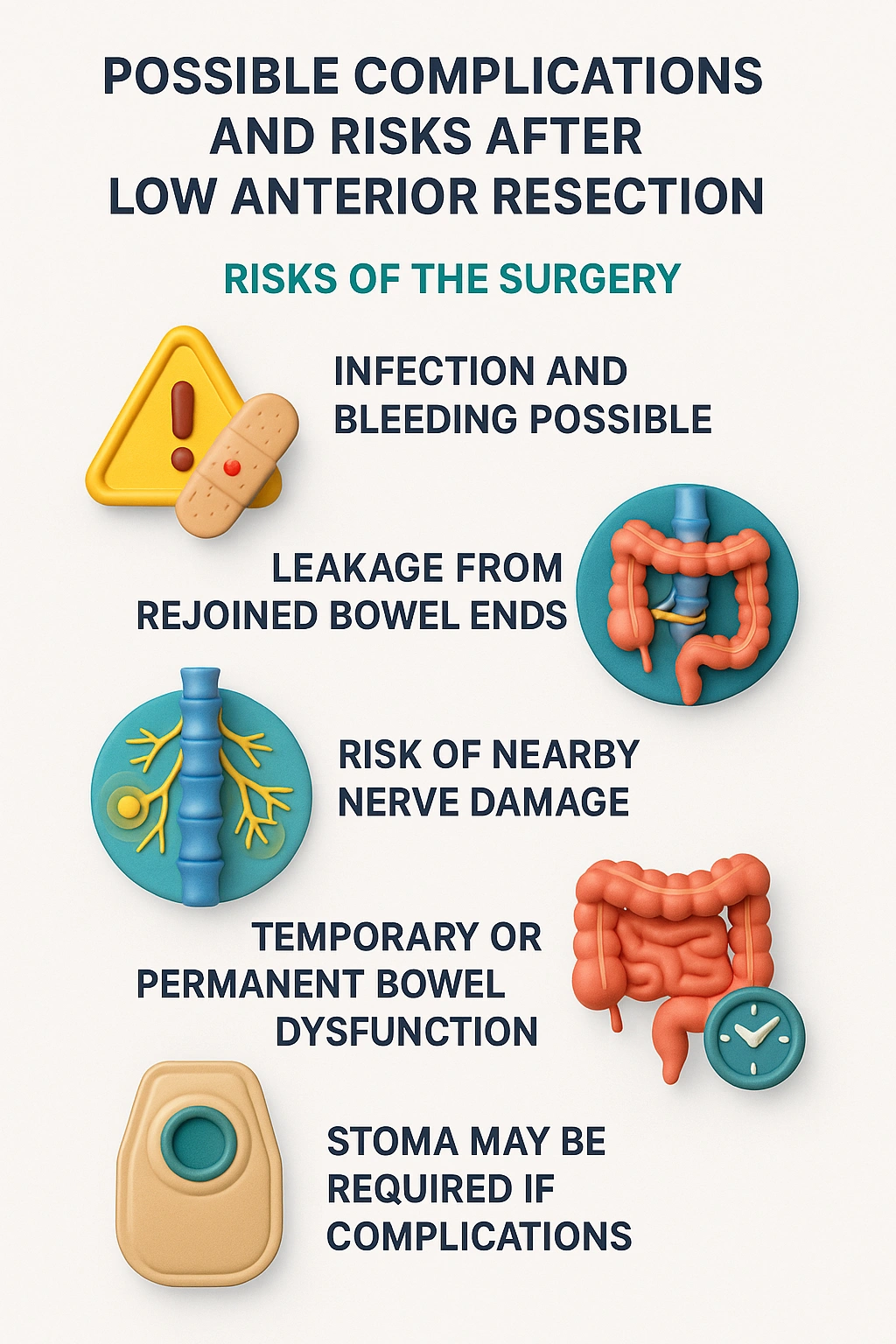
This can lead to problems with urination or, in men, difficulty with erections and ejaculation, and in women, vaginal dryness or pain. These issues often improve with time, but for some, they can be permanent.
- Infection, Bleeding, and Other General Risks
Other general risks associated with any major surgery include:
⦿ Infection at the incision site (wound infection).
⦿ Bleeding during or after surgery.
⦿ Blood clots in the legs (DVT) or lungs (pulmonary embolism).
⦿ Problems related to anaesthesia.
Long-Term Outcomes and Survival Rates
- Local Recurrence and Disease-Free Survival
- Impact on Quality of Life
- Role of Adjuvant Therapy
⦿ Chemotherapy: To kill any cancer cells that may have spread elsewhere in the body.
⦿ Radiation Therapy: Sometimes given before surgery (neoadjuvant) to shrink the tumour and make it easier to remove.
- Comparison with Other Surgical Options
Low Anterior Resection Syndrome (LARS)
- Symptoms of LARS
LARS symptoms can range from mild to severe and can include:
⦿ Frequency: Needing to go to the toilet very often.
⦿ Urgency: A sudden, strong need to rush to the toilet.
⦿ Incontinence: Leaking stool or gas without meaning to.
⦿ Clustering: Needing to pass stool multiple times within a short period (e.g., several times in an hour).
⦿ Incomplete Evacuation: A feeling that you haven’t completely emptied your bowels.
⦿ Alternating constipation and diarrhea.
- Strategies for Management
The good news is that there are many ways to manage LARS, and symptoms often improve over the first one to two years after surgery. Management strategies include:
⦿ Dietary changes: Identifying and avoiding foods that trigger your symptoms.
⦿ Medications: Using anti-diarrheal medicines (like loperamide) or bulking agents (like psyllium husk) to regulate stool consistency.
⦿ Bowel training: Establishing a regular routine for going to the toilet.
⦿ Rectal irrigation: A technique where you use water to wash out the bowel at a scheduled time, which can give you control and prevent accidents for the rest of the day.
- Swipe right to view the full table
| Symptom Group | Dietary Strategies | Lifestyle & Medical Tips |
|---|---|---|
| Frequency & Urgency | Eat small, frequent meals. Avoid caffeine, alcohol, and very spicy foods which can stimulate the bowel. | Plan toilet access. Take anti-diarrheal medication as prescribed before going out. |
| Incontinence / Leakage | Eat foods that thicken stool like bananas, rice, applesauce, toast (BRAT diet), and potatoes. | Practice pelvic floor exercises (Kegels). Use pads for security. Consider rectal irrigation. |
| Incomplete Emptying / Clustering | Ensure adequate fluid and soluble fibre intake to form soft, easy-to-pass stool. | Try different toilet positions (e.g., using a small stool for your feet). Avoid straining. |
- Pelvic Floor Rehabilitation
A physical therapist who specializes in pelvic floor health can be incredibly helpful. They can teach you exercises (like Kegels) to strengthen the pelvic floor and sphincter muscles, which can improve control and reduce incontinence.
- Lifestyle and Diet Modifications
Learning to live with LARS often involves some trial and error. Keeping a food and symptom diary can help you identify your personal triggers. Planning ahead when you go out, knowing where the nearest toilets are, and carrying a small “emergency kit” can reduce anxiety and help you feel more confident. The success of a Low Anterior Resection is not just about removing the cancer but also about managing these long-term effects.
Frequently Asked Questions
Will I Need a Permanent Stoma?
How Long Is Recovery After LAR?
What Are Signs of Complications?
⦿ Fever (high temperature).
⦿ Severe or increasing abdominal pain.
⦿ Redness, swelling, or pus draining from your incisions.
⦿ Nausea, vomiting, or inability to eat or drink.
⦿ No bowel movement or passing of gas for more than 2-3 days.
Can I Live Normally After LAR?
What is a low anterior resection?
What is the definition of low anterior resection?
How does low anterior resection differ from abdominoperineal resection (APR)?
What is the difference between low anterior resection and ultra-low anterior resection?
What is an ultra-low anterior resection?
How does anterior resection differ from low anterior resection?
What are the key differences between ultra-low anterior resection and low anterior resection?
What is shown in a low anterior resection video?

Written by
Dr. Harsh Shah
MS, MCh (G I cancer Surgeon)
Dr. Harsh Shah is a renowned GI and HPB Robotic Cancer Surgeon in Ahmedabad.

Reviewed by
Dr. Swati Shah
MS, DrNB (Surgical Oncology)
Dr. Swati Shah is a Robotic Uro and Gynecological Cancer Surgeon in Ahmedabad.
