Human Papillomavirus (HPV) Testing
What It Detects & Why It’s Important
This guide will explain everything in simple, easy-to-understand language. We will talk about what this test is, why it’s needed, who should get it, and what to expect. Think of this as a friendly conversation about your health, making sure you have all the knowledge to make the best decisions for yourself. Understanding Human Papillomavirus Testing is the first step towards a healthier future.
Summary
- Why HPV Testing Matters
- Who Should Get Tested
- How the Test is Done
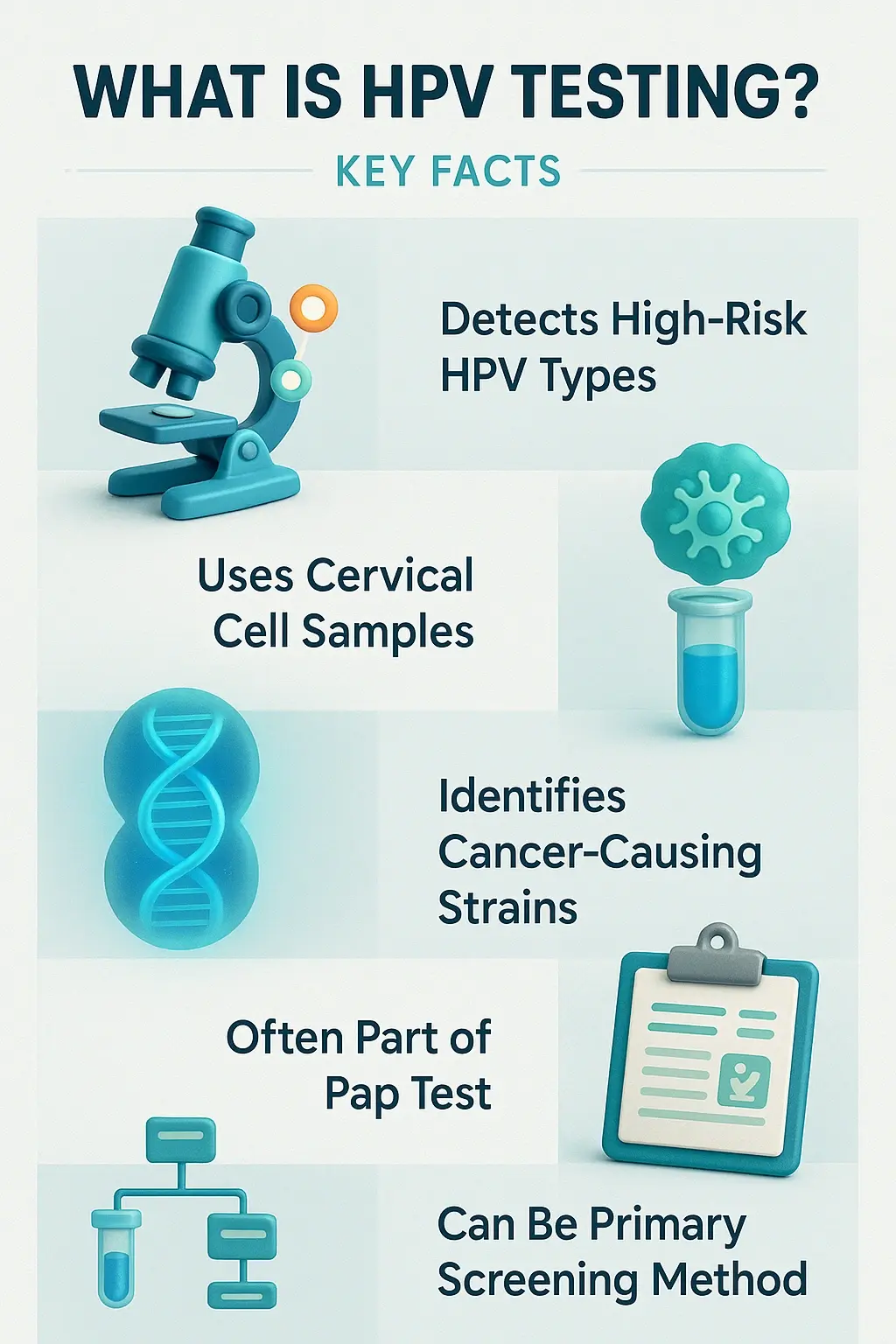
What Is an HPV Test?
- History
- HPV test meaning and purpose
- Difference between HPV test and Pap smear
Many people get confused between an HPV test and a Pap smear (or Pap test). Here’s a simple way to understand it:
⦿ A Pap Smear looks for changes in the cells of your cervix. It checks if the cells look abnormal, which could be an early sign of cancer. Think of it like looking for smoke.
⦿ An HPV Test looks for the virus (HPV) itself, specifically the types that can cause those cell changes. Think of it as looking for the match that could start the fire.
- What types of HPV are detected?
There are more than 100 types of human papillomavirus, but not all of them are human papillomavirus dangerous. They are often grouped into two categories:
⦿ Low-Risk HPV: These types usually cause warts, like human papillomavirus on skin or genital warts, but they rarely lead to cancer.
⦿ High-Risk HPV: These are the ones doctors are most concerned about. There are about 14 high-risk types, with two of them, HPV 16 and HPV 18, being responsible for most HPV-related cancers. The Human Papillomavirus Testing specifically looks for these high-risk strains.
- Here is a table to better understand the human papillomavirus classification.
- Swipe right to view the full table
| Category | Common HPV Types | Associated Health Risks |
|---|---|---|
| High-Risk HPV | HPV 16, 18, 31, 33, 45, 52, 58, and others. | Can cause cervical, anal, oral, and throat cancers. Often show no symptoms until advanced stages. |
| Low-Risk HPV | HPV 6, 11, and others. | Primarily cause genital warts. Rarely associated with cancer. Warts can appear on genitals, anus, mouth, or throat. |
| Common Warts | HPV 2, 7, and others. | Cause common skin warts on hands (like human papillomavirus on finger) and feet (like human papillomavirus warts on feet). |
Who Should Get an HPV Test?
- Women above age 30
- Women with abnormal Pap smear results
- Women with a family history of cervical cancer
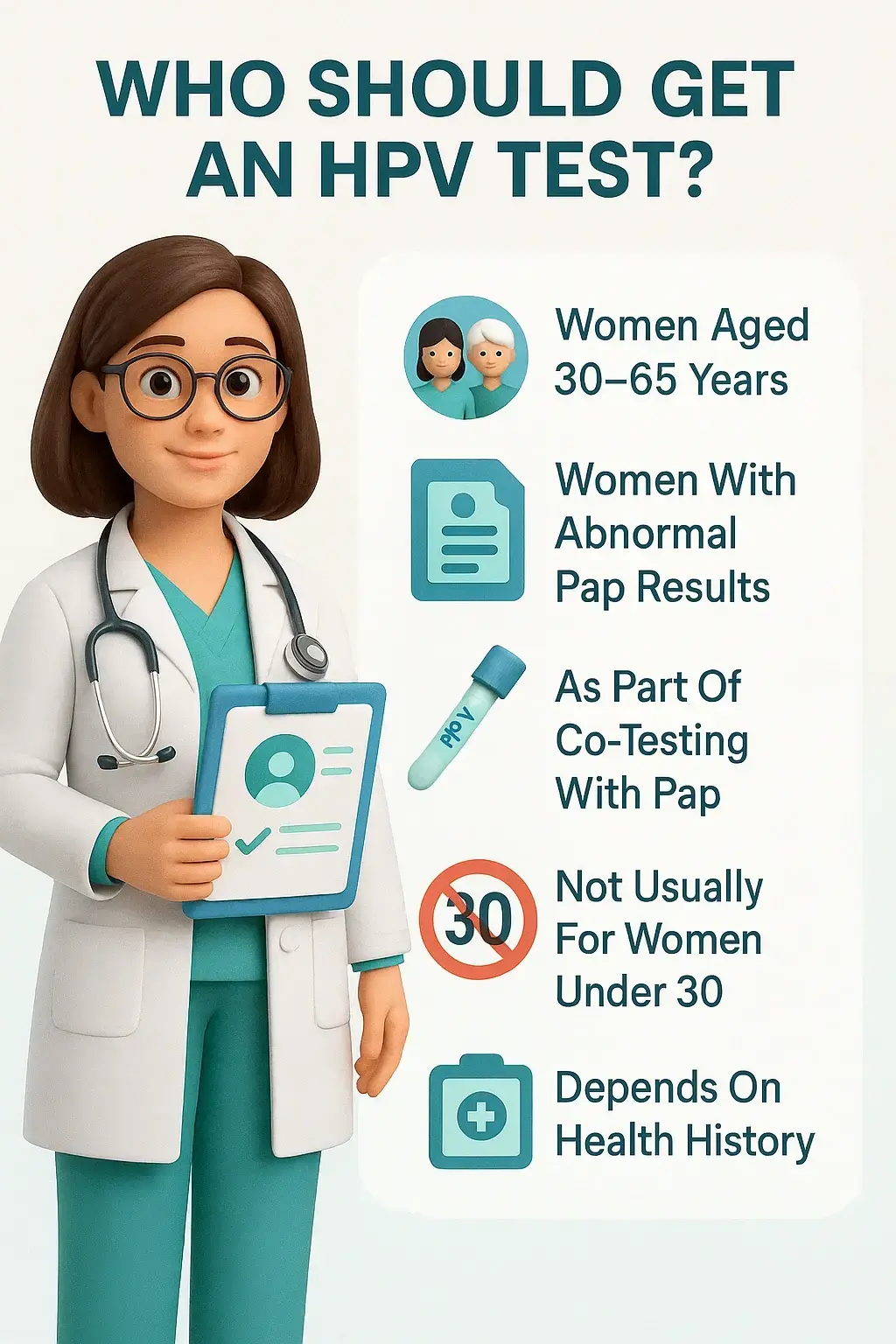
- Guidelines for younger women (under 30)
- Here is a simple table outlining the general screening guidelines.
- Swipe right to view the full table
| Age Group | Recommended Screening Test | Frequency |
|---|---|---|
| Under 21 | No screening recommended. | N/A |
| 21–29 years | Pap Smear only. | Every 3 years. |
| 30–65 years |
Preferred: HPV Test alone or Co-testing (HPV Test + Pap Smear). Acceptable: Pap Smear alone. |
HPV Test every 5 years. Co-testing every 5 years. Pap Smear every 3 years. |
| Over 65 | No screening needed if prior tests were consistently normal. | Discuss with your doctor. |
Types of HPV Tests Available
- HPV DNA test
HPV Test Procedure: What to Expect
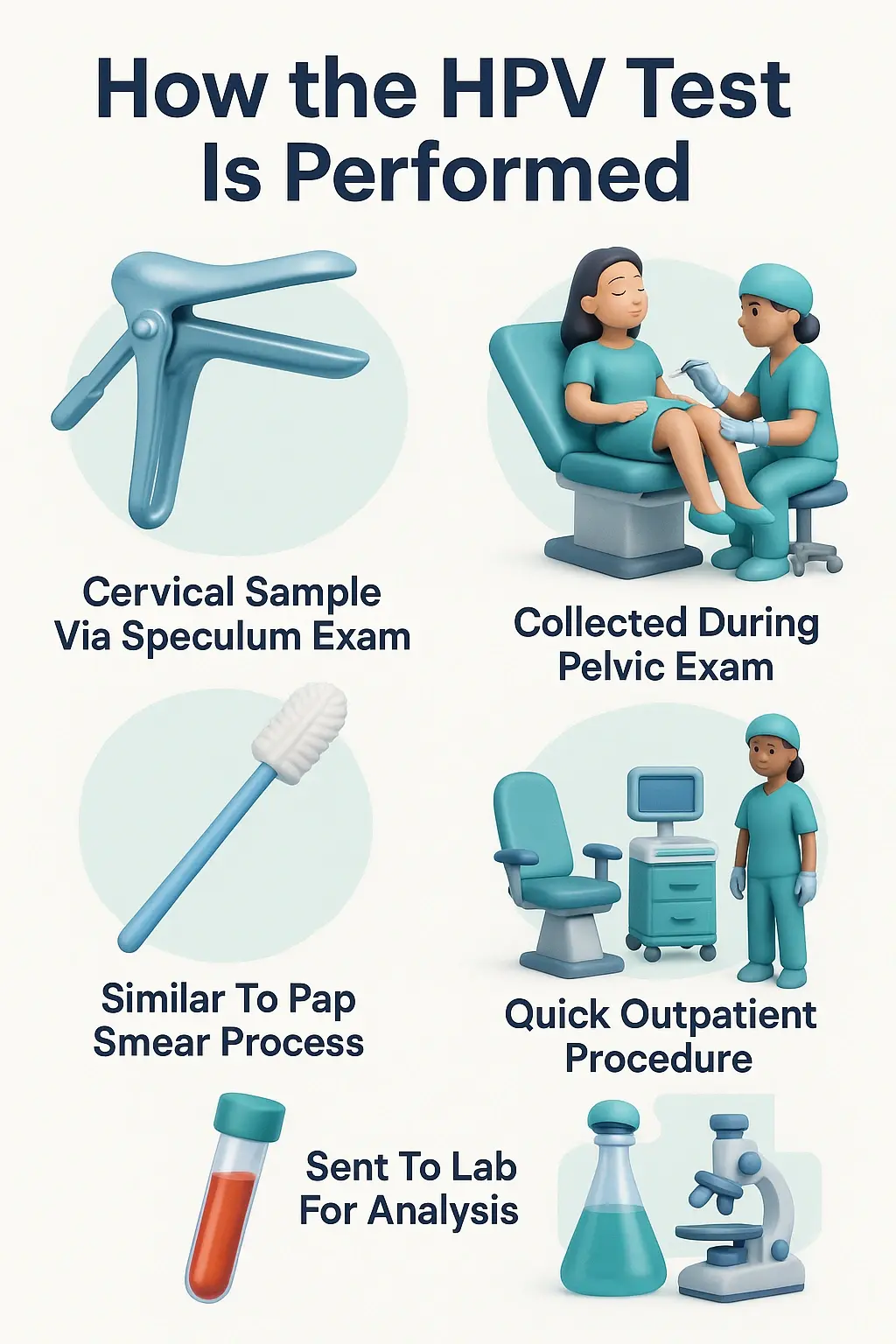
- How cervical cells are collected
⦿ You will be asked to lie on an examination table with your feet placed in supports.
⦿ The doctor will gently insert a small instrument called a speculum into your vagina. This instrument holds the walls of the vagina open so the doctor can clearly see your cervix.
⦿ Using a tiny, soft brush or a small spatula, the doctor will lightly swipe the surface of your cervix to collect a sample of cells.
⦿ The sample is then placed in a special liquid and sent to a laboratory for analysis.
- Precautions before the test
To ensure the test results are as accurate as possible, the lab needs a clear sample of your cervical cells. That’s why there are a few things you should avoid doing right before your appointment for a Human Papillomavirus Testing. We will cover these in the next section. Following these simple precautions is very important for an accurate result.
- Test duration and comfort level
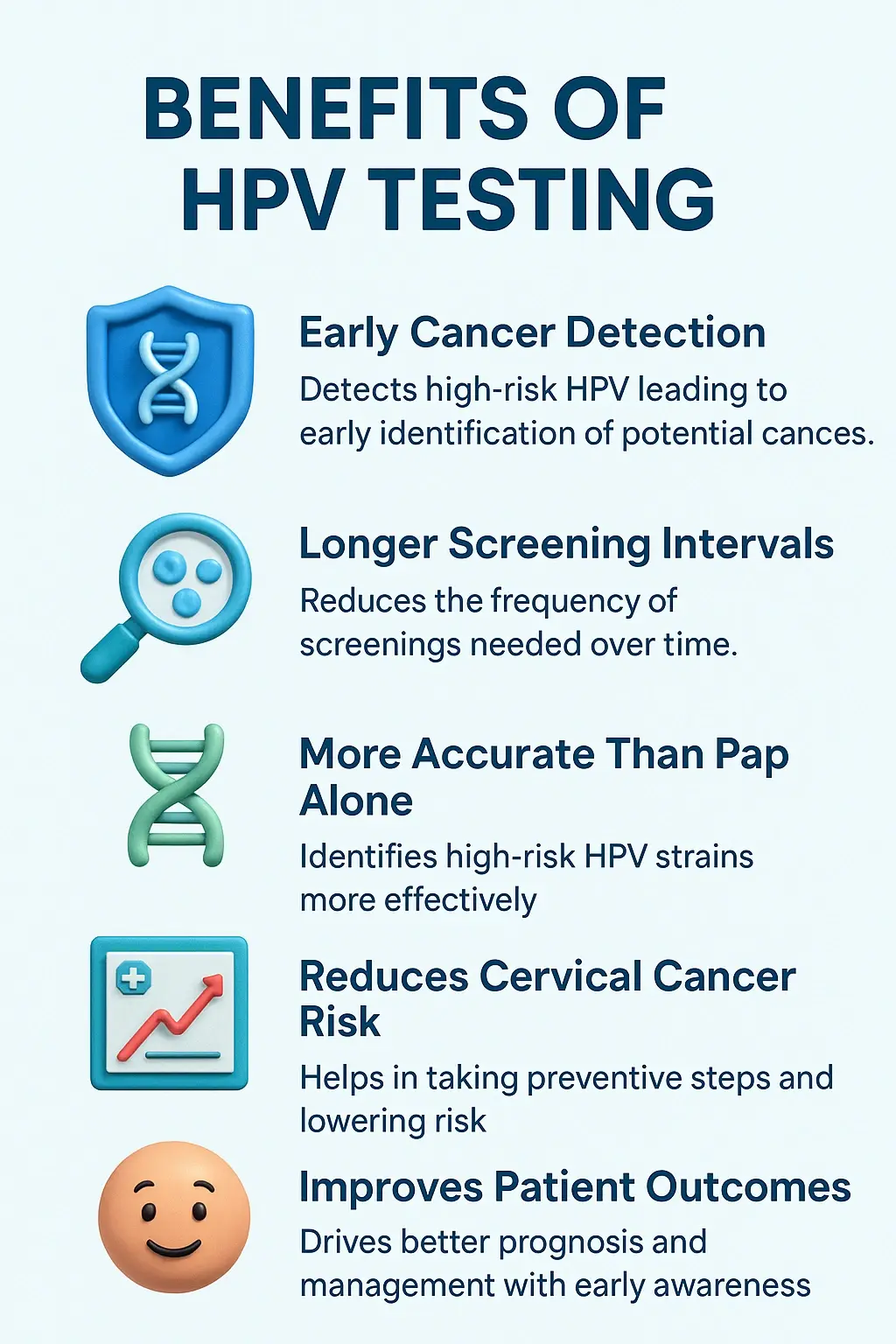
Benefits of HPV Testing
- Prevention comes first
It acts like an early warning system, giving you and your doctor plenty of time to prevent cancer before it ever develops.
- Save time and worry less
This means most women only need to get tested every 5 years instead of every 3 years. This means fewer trips to the clinic and more peace of mind for you.
- Better accuracy for peace of mind
Essentially, think of the Pap smear as looking for smoke (cell changes), while the HPV test looks for the matches (the virus) before the fire can even start.
How to Prepare for an HPV Test
- Avoiding intercourse before the test
- Not using vaginal products 24–48 hours before
For the same reason, you should avoid using any products inside your vagina for 24 to 48 hours before your Human Papillomavirus Testing. This includes:
⦿ Vaginal creams or suppositories
⦿ Spermicidal foams or jellies
⦿ Tampons
⦿ Douching (washing or cleaning out the inside of the vagina with water or other fluids)
These products can wash away or obscure the cervical cells, making the test less reliable.
- Best time to schedule the test
Understanding HPV Test Results
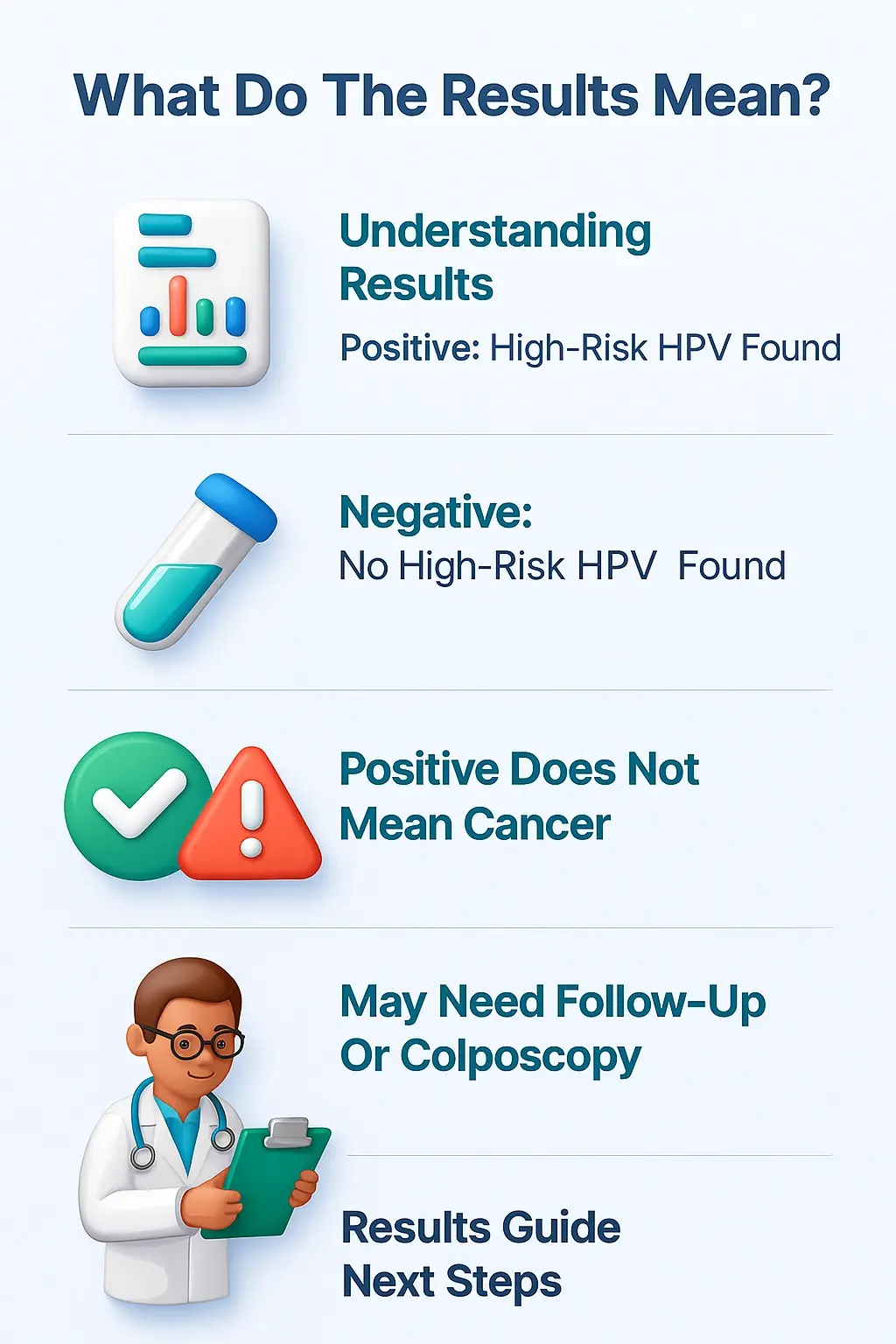
- What a positive result means
- Negative HPV test – what next?
- Women with a family history of cervical cancer
- When further testing or biopsy is needed
If your test is positive, your doctor will decide the next steps based on your age, your specific results (especially if you have HPV 16 or 18), and the results of your Pap smear if you had one. Further steps might include:
⦿ A repeat test in one year: To see if the infection has cleared on its own.
⦿ A colposcopy: A procedure where the doctor uses a special magnifying lens to look closely at your cervix.
⦿ A biopsy: If the doctor sees an abnormal area during the colposcopy, they may take a tiny piece of tissue to be examined under a microscope. This is the only way to confirm the presence of pre-cancerous cells.
- This table helps summarize what your results could mean.
- Swipe right to view the full table
| Test Result | What It Means | Likely Next Step |
|---|---|---|
| HPV Negative | No high-risk HPV was found. Your risk of cervical cancer is very low. | Return for your next routine screening in 5 years. |
| HPV Positive (not 16/18) | A high-risk HPV was found, but not one of the two most common cancer-causing types. | Your doctor may recommend a repeat test in 12 months or a colposcopy. |
| HPV Positive (type 16 or 18) | One of the two highest-risk HPV types was found. | Your doctor will almost certainly recommend a colposcopy to examine your cervix more closely. |
| HPV Positive & Abnormal Pap Smear | A high-risk HPV was found, and your cervical cells already show some changes. | A colposcopy is highly recommended to investigate the cell changes. |
Risks and Limitations of HPV Testing
- False positives or negatives
⦿ False Positive: This is when the test says you have high-risk HPV, but you actually don’t. This can lead to unnecessary anxiety and follow-up procedures.
⦿ False Negative: This is when the test says you do not have high-risk HPV, but you actually do. This is rarer but more serious, as it can give a false sense of security.
However, modern HPV tests are highly accurate, and these instances are not very common.
- Emotional impact of positive result
- Does HPV test detect cancer directly?
HPV Test vs Pap Smear: Key Differences
- Purpose of each test
⦿ Purpose of Pap Smear: To find abnormal or pre-cancerous cells on the cervix. It is a direct look at the health of your cervical cells right now.
⦿ Purpose of Human Papillomavirus Testing: To find the high-risk HPV virus that can cause those abnormal cell changes. It is a look at your risk of developing cell changes in the future.
Essentially, one looks for the effect (abnormal cells), and the other looks for the cause (the virus).
- Frequency of testing recommended
The recommended frequency depends on the test you are having and your age.
⦿ Pap Smear alone: Typically recommended every 3 years for women aged 21-65.
⦿ Human Papillomavirus Testing alone: Recommended every 5 years for women aged 30-65.
⦿ Co-testing (both tests together): Recommended every 5 years for women aged 30-65.
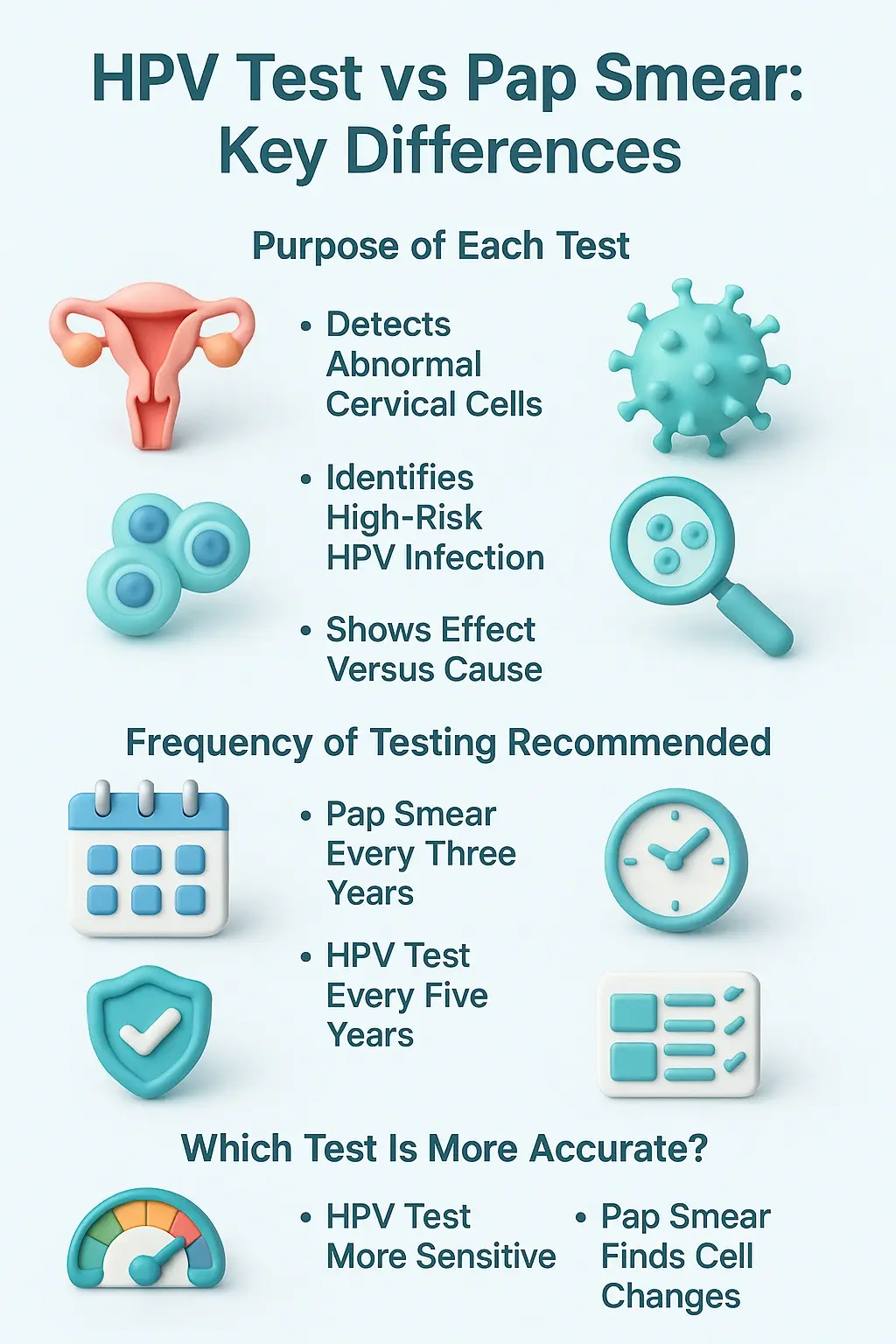
- Which test is more accurate?
HPV Testing in India: Cost & Accessibility
- Average cost in private labs and hospitals
- Urban vs rural accessibility
Frequently Asked Questions
What is human papillomavirus (HPV)?
Can human papillomavirus be cured or treated?
How long does human papillomavirus last in the body?
Does human papillomavirus cause cancer?
How does human papillomavirus cause cancer?
What does human papillomavirus look like?
How many types of human papillomavirus are there?
How common is human papillomavirus worldwide?
Is human papillomavirus the same as herpes?

Written by
Dr. Swati Shah
MS, DrNB (Surgical Oncology)
Dr. Swati Shah is a Robotic Uro and Gynecological Cancer Surgeon in Ahmedabad.

Reviewed by
Dr. Harsh Shah
MS, MCh (G I cancer Surgeon)
Dr. Harsh Shah is a renowned GI and HPB Robotic Cancer Surgeon in Ahmedabad.
