Urinary Bladder Cancer
How Does It Affect Your Daily Life?
Because it can grow slowly without causing many other symptoms at first, there can be a dangerous delay in getting it checked. This guide is here to help you understand the early signs of urinary bladder cancer, how it’s found, and how it can be treated. Knowing what to look for can truly save lives.
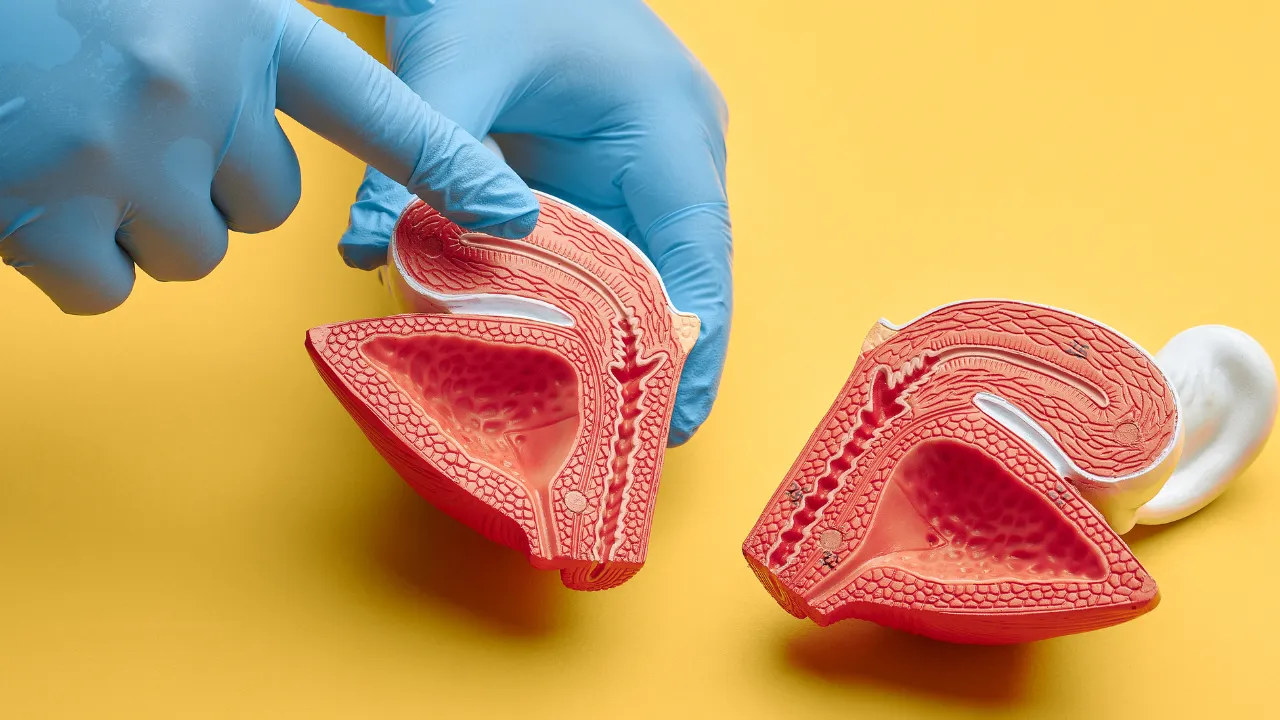
What is Urinary Bladder Cancer?
Urinary bladder cancer happens when bad cells grow in the wall of the bladder. The bladder is a balloon-shaped organ that stores pee from the kidneys until you go to the bathroom. This cancer can be mild and stay in one place or be more serious and spread to other parts of the body.
Have a Question?
Types of Bladder Cancer
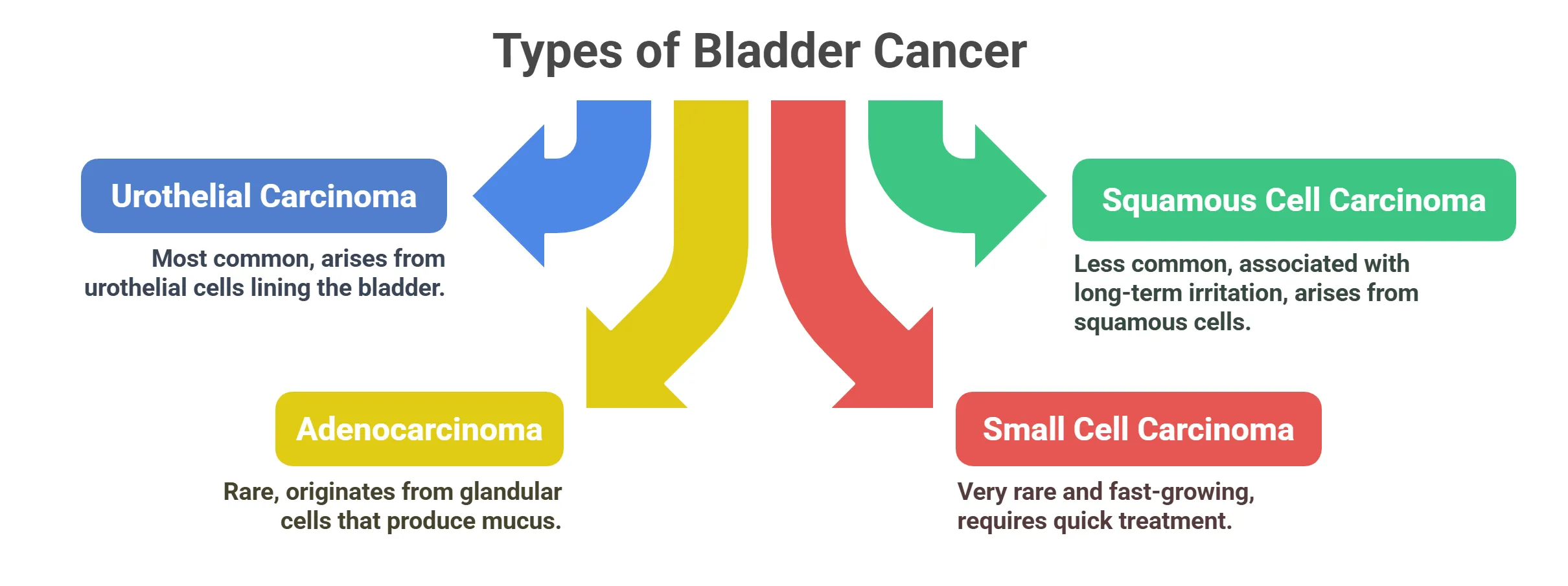
- Urothelial Carcinoma (Transitional Cell Carcinoma)
This is the most common type of bladder cancer. Urothelial cells line the inside of the bladder. This type of cancer starts in these cells. It is also called transitional cell carcinoma.
This type of cancer is less common. It starts in squamous cells, which are flat cells that can form in the bladder lining after long-term infection or irritation.
Adenocarcinoma is a rare type of bladder cancer. It begins in glandular cells in the bladder. These cells make and release mucus.
This is a very rare and fast-growing type of bladder cancer. It starts in small, round cells. It needs to be treated quickly.
Early Signs and Symptoms of Bladder Cancer
- Common Symptoms
Hematuria
(Blood in Urine)
⦿ Microscopic: Sometimes, you can’t see the blood, but a doctor can find it with a test.
⦿ Macroscopic: Other times, you can see the blood, which makes your pee look pink, red, or brown. Even a little blood in your urine should be checked by a doctor.

Painful Urination (Dysuria)
⦿ Burning Sensation: A feeling of burning or stinging when you pass urine, which can be a sign of irritation.
⦿ Pain or Discomfort: Experiencing pain or general discomfort in your bladder area while urinating.
Frequent Urination
⦿ Going More Often: Needing to urinate more frequently than what is usual for you, including throughout the night.
⦿ Urgency: Feeling a sudden and strong urge to urinate, even when your bladder is not full.
Urgent Need to Urinate

Nocturia (Waking Up at Night to Urinate)
- Less Common Symptoms
Lower Back Pain
Have a Question?
Risk Factors for Urinary Bladder Cancer
- Modifiable Risk Factors
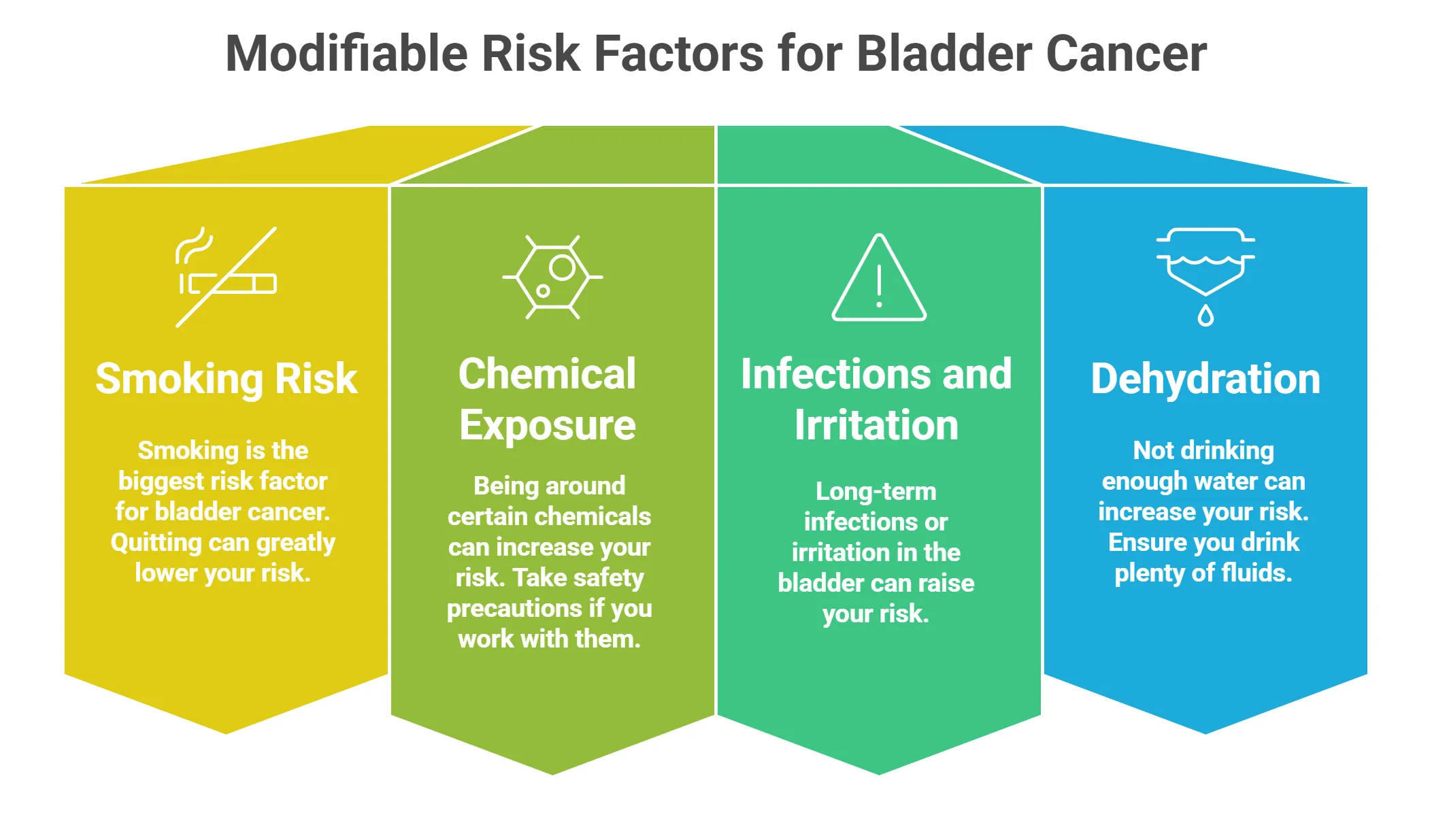
⦿ Smoking: The Leading Cause: Smoking is the biggest risk factor for bladder cancer. If you smoke, quitting can greatly lower your risk.
⦿ Chemical Exposure: Being around certain chemicals can increase your risk.
⦿ Aromatic Amines, Dyes, and Arsenic: These chemicals are used in some jobs. If you work with them, take safety precautions.
⦿ Chronic Bladder Infections and Irritation: Long-term infections or irritation in the bladder can raise your risk.
⦿ Dehydration: Not drinking enough water can also increase your risk. Make sure to drink plenty of fluids.
- Non-Modifiable Risk Factors
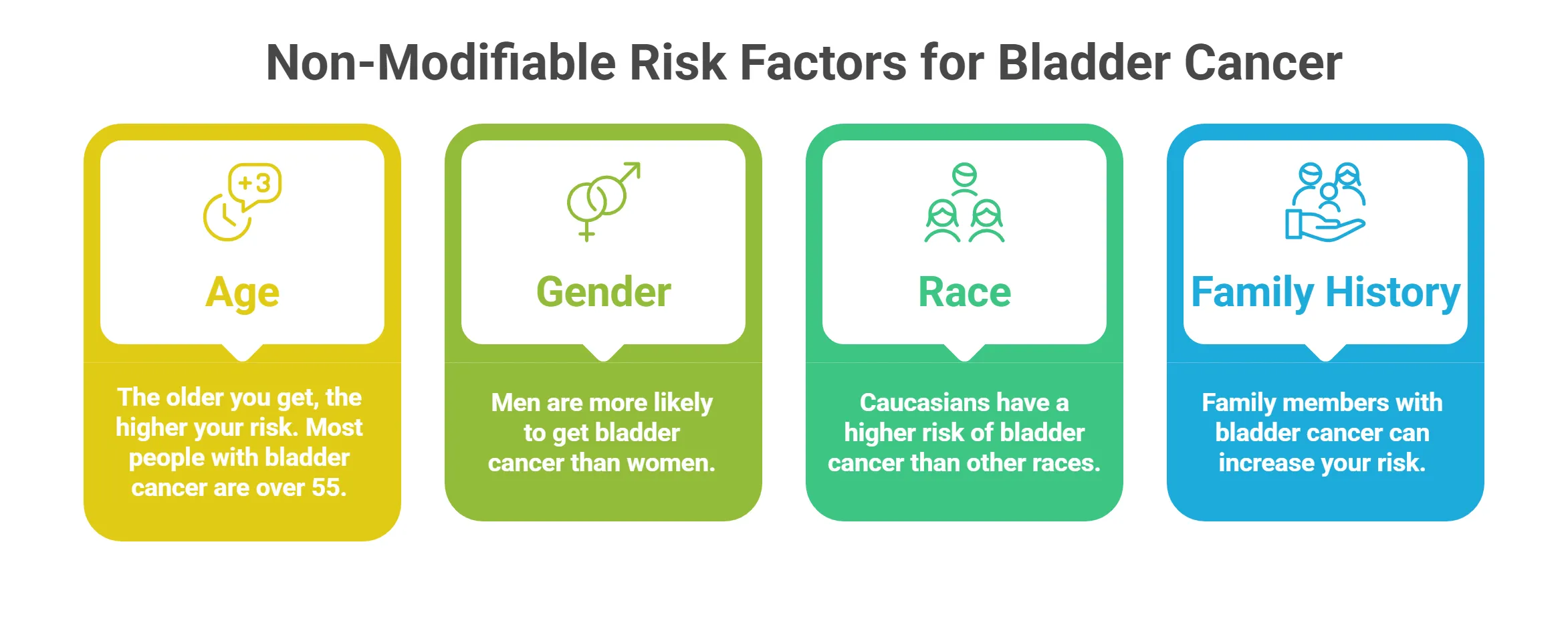
⦿ Age: The older you get, the higher your risk. Most people with bladder cancer are over 55.
⦿ Gender: Men are more likely to get bladder cancer than women.
⦿ Race: Caucasians (white people) have a higher risk of bladder cancer than other races.
⦿ Family History and Genetic Factors: If you have family members who had bladder cancer, your risk might be higher. Some genes can also increase your risk.
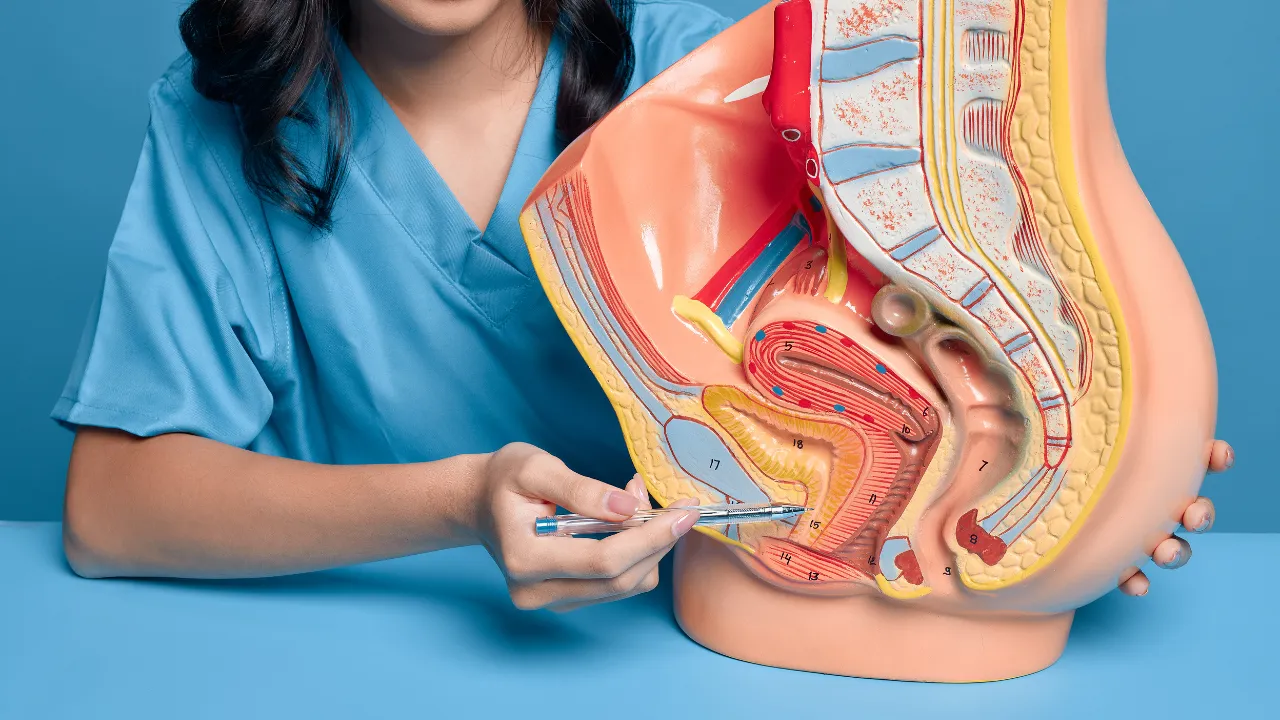
How is Urinary Bladder Cancer Diagnosed?
- Diagnostic Tests
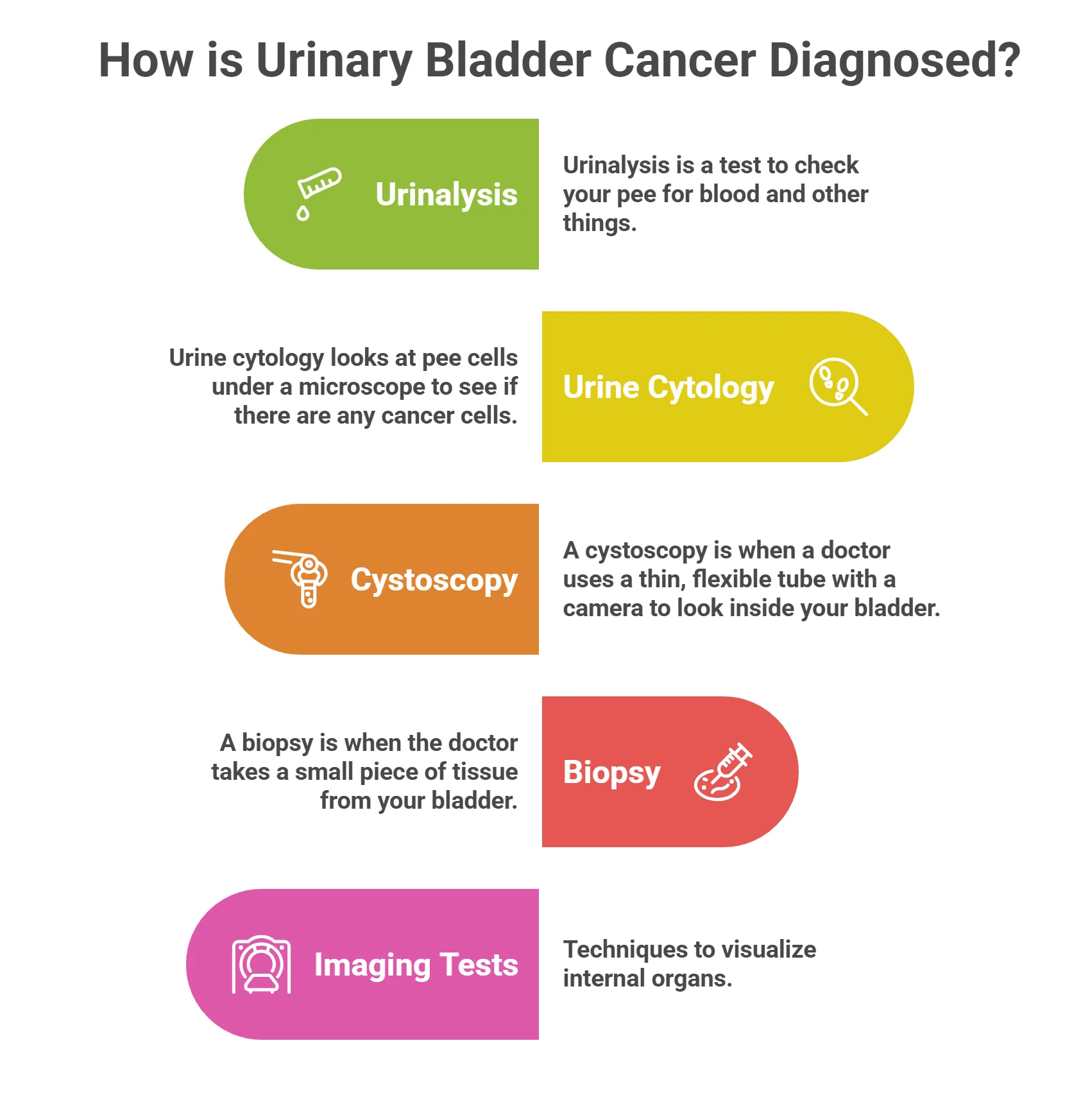
- Urinalysis and Urine Cytology
Urinalysis is a test to check your pee for blood and other things. Urine cytology looks at pee cells under a microscope to see if there are any cancer cells.
- Cystoscopy: Visual Examination of the Bladder
A cystoscopy is when a doctor uses a thin, flexible tube with a camera to look inside your bladder. This helps them see any abnormal areas.
- Biopsy: Confirming Cancer Cells
A biopsy is when the doctor takes a small piece of tissue from your bladder. This tissue is checked under a microscope to see if there are cancer cells. A biopsy is the only way to know for sure if you have bladder cancer.
- Imaging Tests: CT Scans, MRIs, and Ultrasounds
These tests take pictures of your bladder and nearby areas.
⦿ CT scans and MRIs can show if the cancer has spread.
⦿ Ultrasounds use sound waves to create images.
Staging of Bladder Cancer
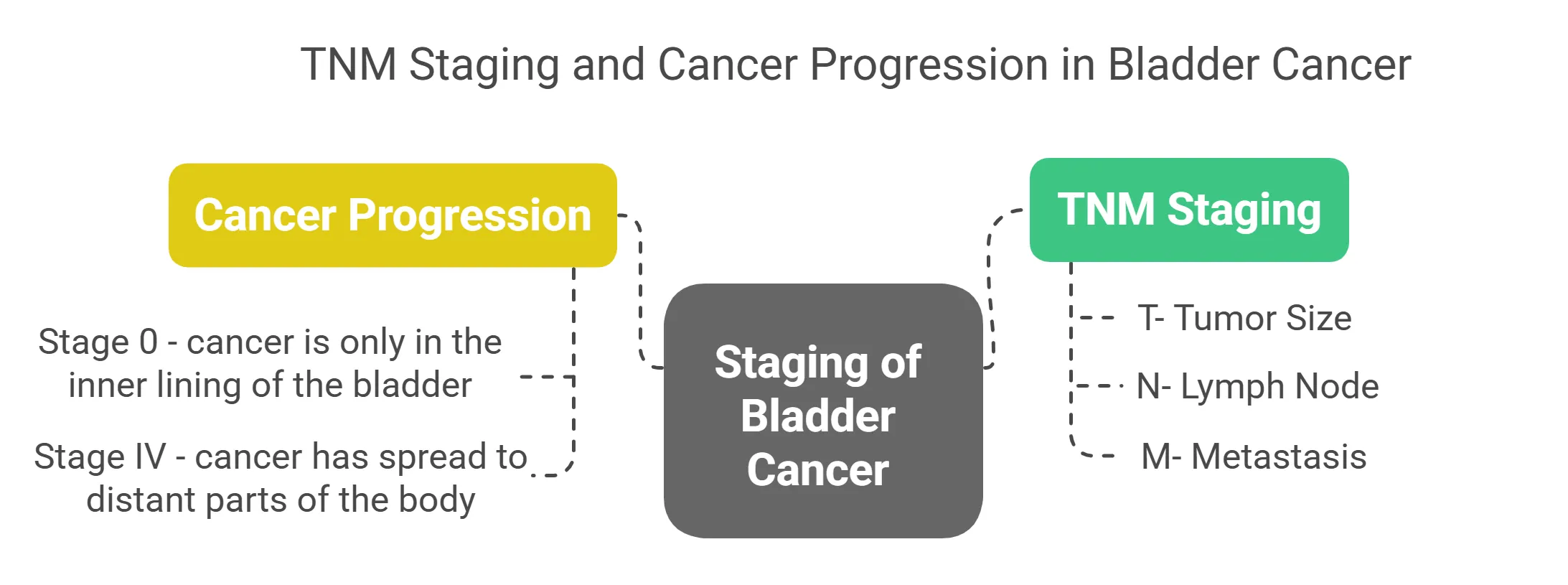
- TNM Staging System: Tumor, Node, Metastasis
⦿ T stands for the size of the tumor.
⦿ N stands for whether the cancer has spread to lymph nodes.
⦿ M stands for whether the cancer has spread to other parts of the body (metastasis).
- Stages 0 to IV: Understanding Cancer Progression
⦿ Stage 0 means the cancer is only in the inner lining of the bladder.
⦿ Stage IV means the cancer has spread to distant parts of the body.
Treatment Options for Urinary Bladder Cancer
- Surgical Treatments
Transurethral Resection of Bladder Tumor (TURBT)
Partial Cystectomy: Removing Part of the Bladder
If the cancer is only in one part of the bladder, the doctor might remove just that part. This is called a partial cystectomy.
Radical Cystectomy: Removing the Entire Bladder
In a radical cystectomy, the doctor removes the entire bladder, as well as nearby lymph nodes and organs. This is done when the cancer has spread or is likely to spread.
Lymph Node Dissection

- Non-Surgical Treatments
Chemotherapy

Chemotherapy uses drugs to kill cancer cells.
⦿ Systemic chemotherapy involves drugs that travel through your whole body.
⦿ Intravesical chemotherapy involves putting drugs directly into your bladder.
Radiation Therapy

Radiation therapy uses high-energy rays to kill cancer cells.
⦿ External beam radiation comes from a machine outside your body.
⦿ Brachytherapy involves putting radioactive materials directly into the tumor.
Immunotherapy

Immunotherapy helps your body’s immune system fight cancer.
⦿ BCG is a type of immunotherapy that is put directly into the bladder.
⦿ Checkpoint inhibitors are drugs that help your immune system recognize and attack cancer cells.
Targeted Therapy

Targeted therapy uses drugs that attack specific parts of cancer cells. This can help stop the cancer from growing and spreading.
- Stage-Wise Treatment Options for Urinary Bladder Cancer
| Cancer Stage | What It Means | Treatment Options |
|---|---|---|
| Stage 0 (Non-invasive) | Cancer is limited to the inner lining of the bladder. |
- TURBT (tumor removal through a scope) - Medicine put directly into the bladder (like BCG) |
| Stage I | Cancer has grown into the inner wall but not into the muscle. |
- TURBT - Bladder medicine therapy - Surgery if not controlled |
| Stage II | Cancer has spread into the bladder muscle. |
- Bladder removal surgery (radical cystectomy) - Chemotherapy before surgery - Sometimes radiation |
| Stage III | Cancer has reached nearby organs or tissues. |
- Surgery to remove bladder and surrounding tissue - Chemotherapy - Radiation in some cases |
| Stage IV (Advanced) | Cancer has spread to distant parts of the body. |
- Chemotherapy - Immunotherapy - Targeted drugs (if suitable) - Supportive care if needed |
Preventing Urinary Bladder Cancer
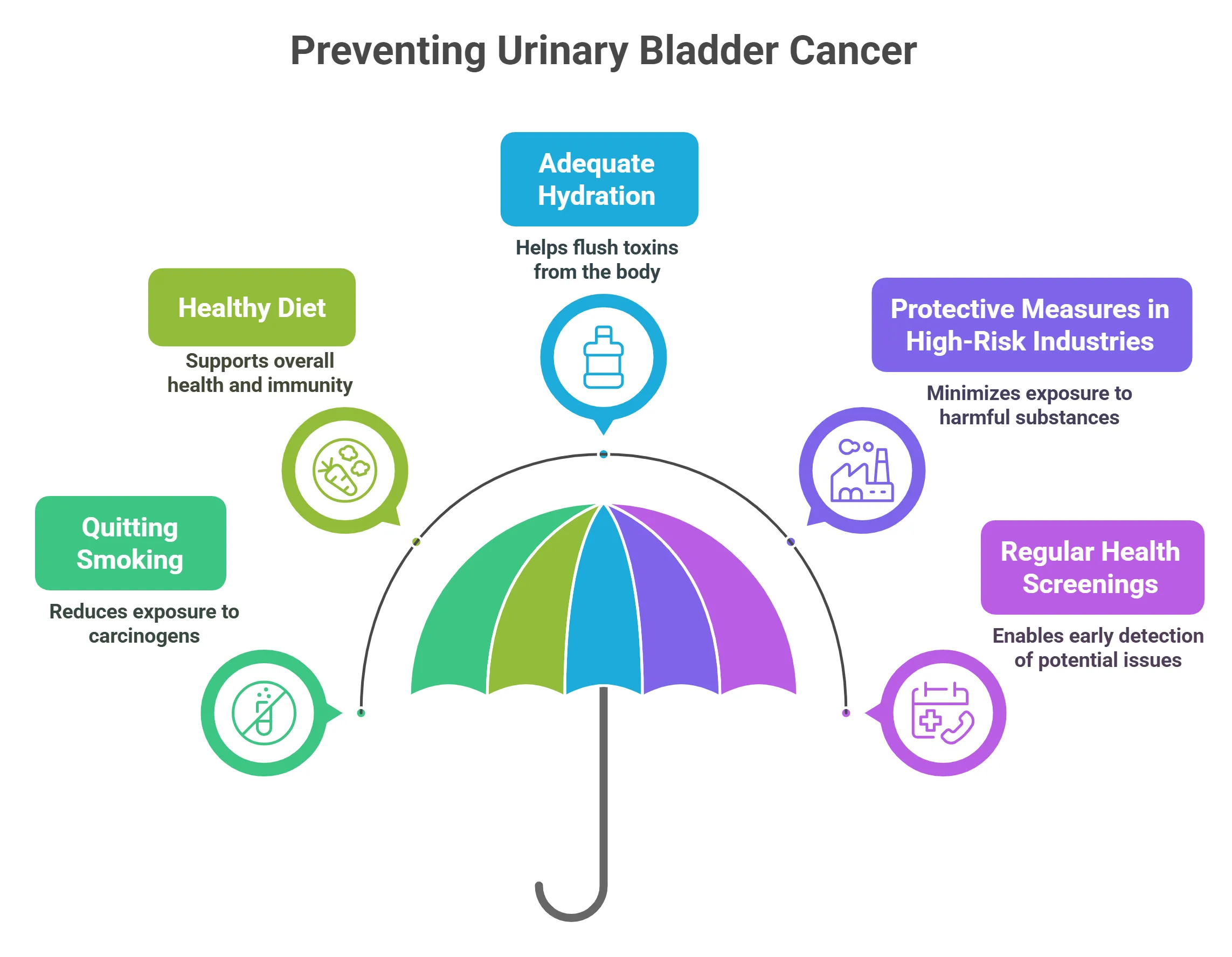
- Lifestyle Changes
⦿ Quitting Smoking: The Most Important Step: Smoking is the biggest risk factor for bladder cancer. Quitting smoking is the most important thing you can do to lower your risk.
⦿ Healthy Diet: Emphasizing Fruits and Vegetables: Eating lots of fruits and vegetables can help protect against bladder cancer. They have vitamins and minerals that keep your body healthy.
⦿ Adequate Hydration: Drinking enough water helps flush out harmful substances from your bladder. Try to drink at least eight glasses of water a day.
- Occupational Safety
⦿ Protective Measures in High-Risk Industries: If you work with chemicals, wear protective gear like gloves and masks. Follow safety rules to avoid exposure.
⦿ Regular Health Screenings: If you work in a high-risk job, get regular check-ups like Screening to look for early signs of cancer.
Have a Question?
Schedule an appointment today!
Frequently Asked Questions
What exactly is urinary bladder cancer?
What are the common symptoms of bladder cancer I should watch out for?
What are the main causes and risk factors for bladder cancer?
How is bladder cancer usually diagnosed?
What are the different stages of bladder cancer, and why do they matter?
What are the primary treatment options available for bladder cancer?
Can bladder cancer be cured, and what factors affect the chances of a cure?
What kind of lifestyle changes can help someone manage or prevent bladder cancer?
Are there any new or experimental treatments for bladder cancer on the horizon?
What should I expect during and after bladder cancer treatment in terms of side effects and recovery?

Written by
Dr. Swati Shah
MS, DrNB (Surgical Oncology)
Dr. Swati Shah is a Robotic Uro and Gynecological Cancer Surgeon in Ahmedabad.

Reviewed by
Dr. Harsh Shah
MS, MCh (G I cancer Surgeon)
Dr. Harsh Shah is a renowned GI and HPB Robotic Cancer Surgeon in Ahmedabad.